BAL Leading the Way Series
“My family knows that after I die, my tissues will be donated to Lyme Disease Biobank to provide researchers with the vital material they need to solve this horrible disease. I urge anyone with chronic/persistent Lyme to register with NDRI today. Let’s end this suffering together.”
-Kirsten Stein, Lyme Advocate
Lyme Disease Biobank®, led by Liz Horn, PhD, MBI, is central to Bay Area Lyme Foundation’s 10-year search for answers to Lyme’s most intractable questions and is the most important program in the Foundation’s mission to make Lyme disease easy to diagnose and simple to cure.
The original Lyme Disease Biobank sample collection launched in 2014 focused on obtaining blood, urine, and serum samples from patients with early/acute Lyme disease. Once this program had been fully established, the Lyme Disease Biobank team explored adding tissue samples to the Biobank. Tissue samples could help researchers expand their investigations beyond the early stage of infection into how chronic/persistent Lyme and other tick-borne diseases impact the central nervous system, joints, and organs of Lyme patients.
With the tissue bank objectives defined, the Biobank connected with specialist organizations to provide the critical support needed to support sample collection and make the development of a tissue bank a reality.
Post-Mortem Tissue Collection Planning
 Lyme Disease Biobank established a key partnership with the nonprofit National Disease Research Interchange (NDRI) to provide logistics for post-mortem tissue collection for the new tissue program. The Biobank also partnered with MyLymeData.org, allowing Lyme patients registered with the Biobank to link their MyLymeData profile to their tissue donation if desired. Bringing these two resources together provides for the organizing and recovery of post-mortem (after death) tissue. It ensures samples include redacted (removes identifying information) detailed patient medical histories—an important nuance for Lyme disease researchers.
Lyme Disease Biobank established a key partnership with the nonprofit National Disease Research Interchange (NDRI) to provide logistics for post-mortem tissue collection for the new tissue program. The Biobank also partnered with MyLymeData.org, allowing Lyme patients registered with the Biobank to link their MyLymeData profile to their tissue donation if desired. Bringing these two resources together provides for the organizing and recovery of post-mortem (after death) tissue. It ensures samples include redacted (removes identifying information) detailed patient medical histories—an important nuance for Lyme disease researchers.
 “Although it is an emotional and difficult idea for anyone to plan to donate parts of their body to science after they have died, we believe that this decision is an important way for Lyme patients to change the course of Lyme disease research. Having access to tissues from the brain, heart, joints, and central nervous system of Lyme patients allows researchers to prove unequivocally that Lyme is present in tissue and contributes to patient suffering,” explains Linda Giampa, Executive Director, Bay Area Lyme Foundation and board member of Lyme Disease Biobank.
“Although it is an emotional and difficult idea for anyone to plan to donate parts of their body to science after they have died, we believe that this decision is an important way for Lyme patients to change the course of Lyme disease research. Having access to tissues from the brain, heart, joints, and central nervous system of Lyme patients allows researchers to prove unequivocally that Lyme is present in tissue and contributes to patient suffering,” explains Linda Giampa, Executive Director, Bay Area Lyme Foundation and board member of Lyme Disease Biobank.
Post-mortem Donation Occurs
The initial donation of post-mortem tissue samples to Lyme Disease Biobank occurred in the fall of 2019 and was the first of several such donations. “Post-mortem donations cause mixed emotions for the team,” comments Liz Horn. “There is great sadness that someone who is part of the Lyme community is gone, but there is also hope that their tissue samples will provide answers for these complex illnesses and reduce future suffering. The post-mortem donation team is acutely aware of—and sensitive to—the struggles of chronic/persistent Lyme patients.”
 Lyme patient, advocate, and member of Bay Area Lyme’s advisory board, Kirsten Stein is registered with NDRI and has already linked her MyLymeData profile to her registration so researchers will be able to access her redacted medical history alongside her tissue samples. Kirsten notes: “My family knows that after I die, my tissues will be donated to Lyme Disease Biobank to provide researchers with the vital material they need to solve this horrible disease. I urge anyone with chronic/persistent Lyme to register with NDRI today. Let’s end this suffering together.”
Lyme patient, advocate, and member of Bay Area Lyme’s advisory board, Kirsten Stein is registered with NDRI and has already linked her MyLymeData profile to her registration so researchers will be able to access her redacted medical history alongside her tissue samples. Kirsten notes: “My family knows that after I die, my tissues will be donated to Lyme Disease Biobank to provide researchers with the vital material they need to solve this horrible disease. I urge anyone with chronic/persistent Lyme to register with NDRI today. Let’s end this suffering together.”
Surgical Tissue Collection Launched
With the post-mortem tissue collection program established, the team turned its attention towards collecting tissue from another important source of material: tissue from surgeries. Patients suffering from Lyme and tick-borne diseases may undergo surgeries that could be due to their Lyme disease—like joint replacements—or surgeries not necessarily connected to their Lyme disease.
Because of legal and logistical requirements, planning for an upcoming surgery is required as tissue collection from surgery must be coordinated with the patient’s surgical team and the hospital or medical center. In some instances, it is possible to acquire tissue after surgery depending on hospital policy and individual circumstances.
A Lyme Patient Donates Multiple Joints
 Lyme disease patient advocate Meghan Bradshaw is someone who has had multiple surgeries and joint replacements as a result of Lyme disease and has donated her tissue to Lyme Disease Biobank’s tissue bank. She urges: “I encourage other patients to consider becoming a donor, whether as a living donor via surgical samples or setting up a future post-mortem donation to the Biobank. The team at NDRI made becoming a living donor a seamless experience coordinating with my surgeons and hospitals each time. Donating to the Biobank will help researchers to understand tick-borne diseases better and lead to breakthroughs in diagnostics and treatments.”
Lyme disease patient advocate Meghan Bradshaw is someone who has had multiple surgeries and joint replacements as a result of Lyme disease and has donated her tissue to Lyme Disease Biobank’s tissue bank. She urges: “I encourage other patients to consider becoming a donor, whether as a living donor via surgical samples or setting up a future post-mortem donation to the Biobank. The team at NDRI made becoming a living donor a seamless experience coordinating with my surgeons and hospitals each time. Donating to the Biobank will help researchers to understand tick-borne diseases better and lead to breakthroughs in diagnostics and treatments.”
“I encourage other patients to consider becoming a donor, whether as a living donor via surgical samples or setting up a future post-mortem donation to the Biobank.”
-Meghan Bradshaw, Lyme Advocate
How is Tissue Collected and What Does it Cost?
NDRI manages the tissue collection process, and NDRI staff are on standby 24/7. In a hospital setting during a planned surgery, NDRI will coordinate directly with your healthcare team to recover the tissue. In the case of somebody who has died, the family will alert NDRI. NDRI and its national network of recovery specialists then coordinate with the funeral home, medical examiner’s office, or hospital team to collect tissue from the deceased.
It’s important to note that Lyme Disease Biobank does not have a whole-body donation program, and only recovers designated tissues. Families will always have their loved one’s body to bury or cremate based on their wishes.
The Biobank covers all costs associated with the coordination of tissue recovery. For post-mortem donation, funeral and cremation costs remain the responsibility of the family. For surgical donations, patients remain responsible for the costs associated with the surgery. To learn more about the process of tissue collection, go to Lyme Disease Biobank’s comprehensive FAQs here.
 What Happens to Tissue After Collection?
What Happens to Tissue After Collection?
When the tissue is collected, it is frozen immediately or “fixed” which means it is chemically stabilized. These two methods support different kinds of analysis. For example, “fixed” samples are used to understand the architecture of the tissue, including looking for pathogens (bacteria, parasites, and viruses) and their location within the tissue. Frozen tissue is often used to look for biomarkers or DNA from a pathogen—i.e. evidence that the pathogen was once there in the tissue. The tissue is then sent to the Biobank’s partner Precision for Medicine. Precision for Medicine stores Biobank samples and sends samples to approved researchers at the Biobank’s request.
What are Researchers Looking for in the Tissue?
Lyme Disease Biobank has assembled a group of researchers to evaluate post-mortem tissue, with a focus on the brain. The brain is an area of focus because many patients with chronic/persistent Lyme disease experience neurocognitive issues and decline. As of this blog publication, the Biobank includes brain tissue from 18 post-mortem donors. Donors range in age from 32–97, with an average age of 67. Two-thirds of donors are men, and one-third are women.
The following researchers are key members of the team evaluating Lyme Disease Biobank tissue:
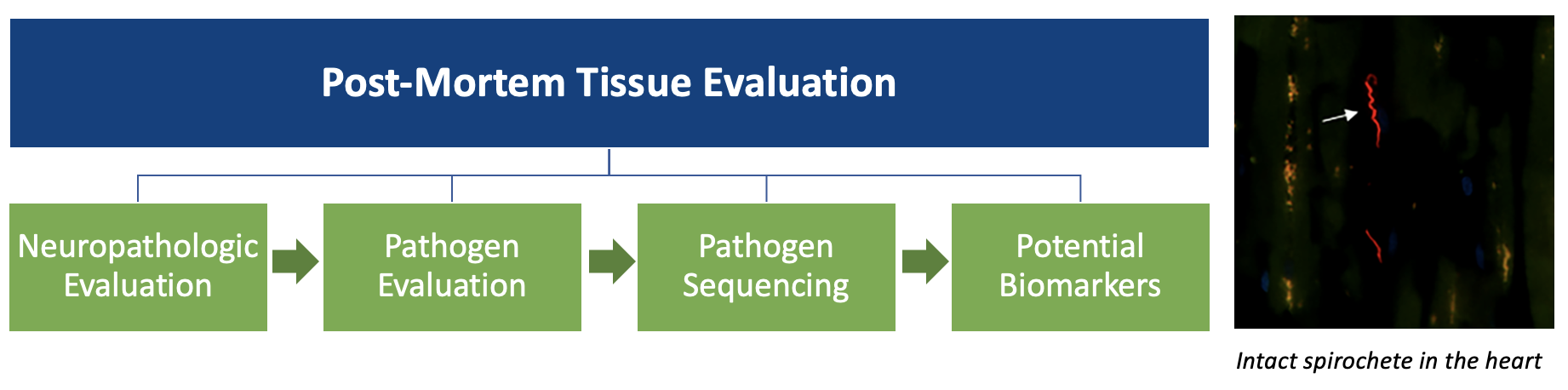
Andrew Dwork , MD, a neuropathologist at Columbia University, reviews the brain tissue, looking for structural abnormalities, evidence of inflammation, and evidence of neurodegenerative diseases such as Alzheimer’s, Parkinson’s, and dementia, among others. Dr. Dwork then writes a specific description of his analysis of the brain, called a neuropathology report, detailing his findings. This report is made available to other researchers who are evaluating samples from the same brain.
, MD, a neuropathologist at Columbia University, reviews the brain tissue, looking for structural abnormalities, evidence of inflammation, and evidence of neurodegenerative diseases such as Alzheimer’s, Parkinson’s, and dementia, among others. Dr. Dwork then writes a specific description of his analysis of the brain, called a neuropathology report, detailing his findings. This report is made available to other researchers who are evaluating samples from the same brain.
 Dr. Monica Embers, a scientist at Tulane University evaluates tissue for pathogens including Borrelia burgdorferi, the bacteria that causes Lyme disease. Dr. Embers and her team use the neuropathology report created by Dr. Dwork as a roadmap to look for pathogens in the brain.
Dr. Monica Embers, a scientist at Tulane University evaluates tissue for pathogens including Borrelia burgdorferi, the bacteria that causes Lyme disease. Dr. Embers and her team use the neuropathology report created by Dr. Dwork as a roadmap to look for pathogens in the brain.
Tissues with evidence of inflammation or disease are then sent to additional approved researchers to confirm the findings. Researchers also evaluate the tissue for biomarkers from the patient or the bacteria. This team of dedicated researchers across seven labs is helping us to understand what happens to tissue in patients infected with tick-borne diseases.
A Family’s Tragedy Leads to Important Findings about Tick-Borne Infections
The first paper, Late-Stage Borreliosis and Substance Abuse, documenting findings from a Biobank post-mortem donation was published in May of 2024. The report focuses on a young man who had multiple tick bites as a child/young adult and a history of increasing tick-borne disease symptoms. Diagnosis and treatment were delayed. He experimented with multiple substances, which tragically led to a homicide-suicide event.

The young man’s tissues were analyzed through the Lyme Disease Biobank tissue program by Dr. Dwork, Dr. Embers, and colleagues. The team found spirochetes in his heart and pancreas, and brain inflammation, suggesting changes in brain biochemistry. A key takeaway from this research is that screening patients who have substance abuse disorders for tick-borne illnesses and appropriately treating these infections may help reduce substance abuse-related deaths, particularly in endemic areas. “We are deeply grateful to the families of Lyme patients, such as this young man, who understood the importance of tissue donation that will increase our understanding and lead to future breakthroughs for patients,” adds Dr. Liz Horn.
A Decade of Development Now Yielding Results
Ten years into the Biobank project, Liz Horn reflects: “We started the Biobank by collecting blood and urine samples. Next, we built a program to collect tissue. Now we are expanding the team of researchers to analyze this tissue and are seeing results. This team will continue to evaluate each tissue donation and share the results with the Lyme and research communities. We are so grateful to the individuals and families who have donated tissue to this resource. This would not be possible without these tissue donations.” The Biobank continues to enroll people interested in donating tissue.
“We are confident that providing human tissue samples to investigators working on better diagnostics and new treatments for Lyme and tick-borne diseases will yield the answers that Lyme patients so desperately need.”
– Linda Giampa, Executive Director, Bay Area Lyme Foundation
In short, the act of donating human tissue that would otherwise be discarded (in the case of surgery), or interred or cremated (in the case of death) is a decision that only each person can make for themselves, usually after consulting their family, or medical provider for surgical donation. For Bay Area Lyme and Lyme Disease Biobank however, there is no doubt that the planning of tissue donations by Lyme patients is a critical—if not ultimately game-changing decision—that will move research forward, and measurably impact our understanding of Lyme and tick-borne diseases.
Linda Giampa, Executive Director of Bay Area Lyme Foundation notes: “We are confident that providing human tissue samples to investigators working on better diagnostics and new treatments for Lyme and tick-borne diseases will yield the answers that Lyme patients so desperately need.”
We would like to recognize and thank the Steven & Alexandra Cohen Foundation, an anonymous donor, the LaureL STEM Fund, and the 2014, 2018, and 2023 LymeAid® Fund-a-Need supporters who have contributed significantly to Lyme Disease Biobank. We are deeply grateful to the participants and families who volunteered and donated samples. If you wish to register as a tissue donor or learn more about the program, please click here. This blog is part of our BAL Leading the Way series. If you require a copy of this article in a bigger typeface and/or double-spaced layout, contact us here. Bay Area Lyme Foundation provides reliable, fact-based information about Lyme and tick-borne diseases so that prevention and the importance of early treatment are common knowledge. For more information about Bay Area Lyme, including our research and prevention programs, go to www.bayarealyme.org. Liz Horn PhD, MDI, serves as PI of Lyme Disease Biobank, a resource created to provide much-needed blood, urine, and tissue samples to researchers studying Lyme disease and other tick-borne infections. More than 1250 participants (representing early Lyme, later stages of Lyme, chronic/persistent Lyme, and controls) have been enrolled. Each participant’s sample donation can support up to 50 different research projects. Currently, 100+ projects in academia and industry have been approved for samples. Liz earned her doctorate in molecular pharmacology and cancer therapeutics from SUNY at Buffalo, was a National Library of Medicine fellow in biomedical informatics, and received her MBI from Oregon Health & Science University. She has spent 2 decades working with non-profit organizations to build research initiatives and collaborations with academia, other non-profits, and industry. Liz is passionate about building resources to move research forward that helps people, improves lives, and reduces suffering. To contact Liz, please email her at info@lymebiobank.org
Liz Horn PhD, MDI, serves as PI of Lyme Disease Biobank, a resource created to provide much-needed blood, urine, and tissue samples to researchers studying Lyme disease and other tick-borne infections. More than 1250 participants (representing early Lyme, later stages of Lyme, chronic/persistent Lyme, and controls) have been enrolled. Each participant’s sample donation can support up to 50 different research projects. Currently, 100+ projects in academia and industry have been approved for samples. Liz earned her doctorate in molecular pharmacology and cancer therapeutics from SUNY at Buffalo, was a National Library of Medicine fellow in biomedical informatics, and received her MBI from Oregon Health & Science University. She has spent 2 decades working with non-profit organizations to build research initiatives and collaborations with academia, other non-profits, and industry. Liz is passionate about building resources to move research forward that helps people, improves lives, and reduces suffering. To contact Liz, please email her at info@lymebiobank.org
