BAL Leading the Way Series
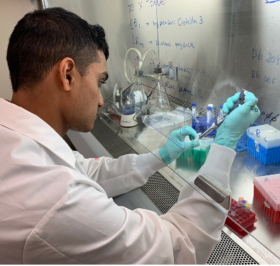
 Sunjya Schweig, MD, founder of the California Center for Functional Medicine, discusses a new program he is developing with funding from Bay Area Lyme to provide education and awareness about Lyme disease and the risks of tick-borne infections for firefighters. Firefighters have a profile of unique occupational exposures, including tick bites, and there is a significant lack of education on this topic. This new program aims to create professional, engaging videos featuring firefighters sharing their experiences and providing information on tick bite prevention, checking for ticks, and what to do if bitten. The goal is to roll out the program in California first, targeting professional firefighter and first responder organizations and eventually expanding nationwide. The exact number of firefighters living with Lyme disease is unknown, but it is acknowledged that they have both occupational and recreational exposures. This new program is seen as a way to bring awareness and education to this population and beyond.
Sunjya Schweig, MD, founder of the California Center for Functional Medicine, discusses a new program he is developing with funding from Bay Area Lyme to provide education and awareness about Lyme disease and the risks of tick-borne infections for firefighters. Firefighters have a profile of unique occupational exposures, including tick bites, and there is a significant lack of education on this topic. This new program aims to create professional, engaging videos featuring firefighters sharing their experiences and providing information on tick bite prevention, checking for ticks, and what to do if bitten. The goal is to roll out the program in California first, targeting professional firefighter and first responder organizations and eventually expanding nationwide. The exact number of firefighters living with Lyme disease is unknown, but it is acknowledged that they have both occupational and recreational exposures. This new program is seen as a way to bring awareness and education to this population and beyond.
“Lyme is not really on the radar for many firefighters. They may have had tick bites either in the line of duty or out mountain biking or hiking when they’re off duty, but many don’t know that tick-borne disease is a big problem.”
– Sunjya Schweig, MD









 The
The