By Bay Area Lyme Foundation BAL Leading the Way Series
“My family knows that after I die, my tissues will be donated to Lyme Disease Biobank to provide researchers with the vital material they need to solve this horrible disease. I urge anyone with chronic/persistent Lyme to register with NDRI today. Let’s end this suffering together.”
-Kirsten Stein, Lyme Advocate
Lyme Disease Biobank®, led by Liz Horn, PhD, MBI, is central to Bay Area Lyme Foundation’s 10-year search for answers to Lyme’s most intractable questions and is the most important program in the Foundation’s mission to make Lyme disease easy to diagnose and simple to cure.
The original Lyme Disease Biobank sample collection launched in 2014 focused on obtaining blood, urine, and serum samples from patients with early/acute Lyme disease. Once this program had been fully established, the Lyme Disease Biobank team explored adding tissue samples to the Biobank. Tissue samples could help researchers expand their investigations beyond the early stage of infection into how chronic/persistent Lyme and other tick-borne diseases impact the central nervous system, joints, and organs of Lyme patients.
With the tissue bank objectives defined, the Biobank connected with specialist organizations to provide the critical support needed to support sample collection and make the development of a tissue bank a reality.
Post-Mortem Tissue Collection Planning
 Lyme Disease Biobank established a key partnership with the nonprofit National Disease Research Interchange (NDRI) to provide logistics for post-mortem tissue collection for the new tissue program. The Biobank also partnered with MyLymeData.org, allowing Lyme patients registered with the Biobank to link their MyLymeData profile to their tissue donation if desired. Bringing these two resources together provides for the organizing and recovery of post-mortem (after death) tissue. It ensures samples include redacted (removes identifying information) detailed patient medical histories—an important nuance for Lyme disease researchers.
Lyme Disease Biobank established a key partnership with the nonprofit National Disease Research Interchange (NDRI) to provide logistics for post-mortem tissue collection for the new tissue program. The Biobank also partnered with MyLymeData.org, allowing Lyme patients registered with the Biobank to link their MyLymeData profile to their tissue donation if desired. Bringing these two resources together provides for the organizing and recovery of post-mortem (after death) tissue. It ensures samples include redacted (removes identifying information) detailed patient medical histories—an important nuance for Lyme disease researchers.
 “Although it is an emotional and difficult idea for anyone to plan to donate parts of their body to science after they have died, we believe that this decision is an important way for Lyme patients to change the course of Lyme disease research. Having access to tissues from the brain, heart, joints, and central nervous system of Lyme patients allows researchers to prove unequivocally that Lyme is present in tissue and contributes to patient suffering,” explains Linda Giampa, Executive Director, Bay Area Lyme Foundation and board member of Lyme Disease Biobank.
“Although it is an emotional and difficult idea for anyone to plan to donate parts of their body to science after they have died, we believe that this decision is an important way for Lyme patients to change the course of Lyme disease research. Having access to tissues from the brain, heart, joints, and central nervous system of Lyme patients allows researchers to prove unequivocally that Lyme is present in tissue and contributes to patient suffering,” explains Linda Giampa, Executive Director, Bay Area Lyme Foundation and board member of Lyme Disease Biobank.
 Our Ticktective host, Dana Parish, interviews Dr. Neil Nathan, renowned physician and best-selling author. Dr. Nathan specializes in treating chronic illnesses, particularly those related to environmental toxins, vector-borne infections, and complex systemic disorders. With decades of experience in clinical practice, he focuses on understanding the impact of toxins on health and is dedicated to helping patients recover from illnesses that conventional medicine often struggles to address. His bestselling book, Toxic: Heal Your Body from Mold Toxicity, Lyme Disease, Multiple Chemical Sensitivities, and Other Chronic Environmental Illnesses, provides a comprehensive guide to recognizing, diagnosing, and treating various chronic conditions linked to environmental factors.
Our Ticktective host, Dana Parish, interviews Dr. Neil Nathan, renowned physician and best-selling author. Dr. Nathan specializes in treating chronic illnesses, particularly those related to environmental toxins, vector-borne infections, and complex systemic disorders. With decades of experience in clinical practice, he focuses on understanding the impact of toxins on health and is dedicated to helping patients recover from illnesses that conventional medicine often struggles to address. His bestselling book, Toxic: Heal Your Body from Mold Toxicity, Lyme Disease, Multiple Chemical Sensitivities, and Other Chronic Environmental Illnesses, provides a comprehensive guide to recognizing, diagnosing, and treating various chronic conditions linked to environmental factors.


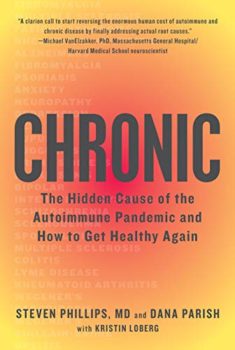 Ticktective host, Dana Parish, talks with her longtime collaborator and co-author of
Ticktective host, Dana Parish, talks with her longtime collaborator and co-author of 


 “I want to leave you with hope. I think we’re going to be unstoppable because I think that these are solvable problems. These are answerable questions. I think that there are already a lot of existing tools in immunology that just need to be brought into the fight, and we can change this.”
“I want to leave you with hope. I think we’re going to be unstoppable because I think that these are solvable problems. These are answerable questions. I think that there are already a lot of existing tools in immunology that just need to be brought into the fight, and we can change this.” 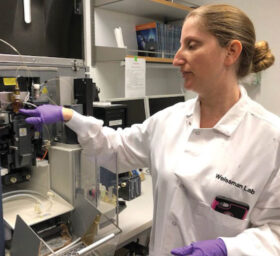 Any respectable pathogen that can establish a persistent infection needs to figure out your immune system to the point that it can evade it. The fact that it has persisted means that it was able to evade your immune clearance. And so, I got to that from a very interesting direction working on immune regulation, trying to understand these brakes on the immune response and how they impact the response to infection. The immune system has the power to kill you and obviously, nobody has any incentive for that to happen. So, there are a lot of mechanisms in place to put brakes on the immune system and reign it in. One of the huge developments in cancer over the last two decades has been reevaluating the question: can we take those brakes off? So in my postdoc, I was studying a particular checkpoint where this was turning into an exciting immuno-oncology target, and I said, ‘I want to look at how this checkpoint is used in infection.’ I realized that this checkpoint was being used to help you survive an acute infection, but created a vulnerability for pathogens to evade immune clearance and establish chronic infection much like it allows cancer cells to evade immune clearance. In an amazing collaboration with Irv Weissman, Balyn Zaro, and Jenifer Coburn we realized that the bacteria that cause Lyme disease manipulate this brake and that’s how I became fascinated with Lyme. But I also became concerned about turning off this brake in cancer patients because I was concerned about what would happen if you used this on cancer patients during an active infection. Indeed, the
Any respectable pathogen that can establish a persistent infection needs to figure out your immune system to the point that it can evade it. The fact that it has persisted means that it was able to evade your immune clearance. And so, I got to that from a very interesting direction working on immune regulation, trying to understand these brakes on the immune response and how they impact the response to infection. The immune system has the power to kill you and obviously, nobody has any incentive for that to happen. So, there are a lot of mechanisms in place to put brakes on the immune system and reign it in. One of the huge developments in cancer over the last two decades has been reevaluating the question: can we take those brakes off? So in my postdoc, I was studying a particular checkpoint where this was turning into an exciting immuno-oncology target, and I said, ‘I want to look at how this checkpoint is used in infection.’ I realized that this checkpoint was being used to help you survive an acute infection, but created a vulnerability for pathogens to evade immune clearance and establish chronic infection much like it allows cancer cells to evade immune clearance. In an amazing collaboration with Irv Weissman, Balyn Zaro, and Jenifer Coburn we realized that the bacteria that cause Lyme disease manipulate this brake and that’s how I became fascinated with Lyme. But I also became concerned about turning off this brake in cancer patients because I was concerned about what would happen if you used this on cancer patients during an active infection. Indeed, the 
 Lyme Disease Biobank established a key partnership with the nonprofit
Lyme Disease Biobank established a key partnership with the nonprofit  “Although it is an emotional and difficult idea for anyone to plan to donate parts of their body to science after they have died, we believe that this decision is an important way for Lyme patients to change the course of Lyme disease research. Having access to tissues from the brain, heart, joints, and central nervous system of Lyme patients allows researchers to prove unequivocally that Lyme is present in tissue and contributes to patient suffering,” explains
“Although it is an emotional and difficult idea for anyone to plan to donate parts of their body to science after they have died, we believe that this decision is an important way for Lyme patients to change the course of Lyme disease research. Having access to tissues from the brain, heart, joints, and central nervous system of Lyme patients allows researchers to prove unequivocally that Lyme is present in tissue and contributes to patient suffering,” explains 
