FOR IMMEDIATE RELEASE
New Bay Area Lyme Foundation Study Reports That Only One-Third of Early Lyme Patients with On-Going Symptoms Followed up with their Healthcare Providers
The new research, published in Frontiers in Medicine, points to need for greater follow-up from medical professionals to address potential treatment failures.
PORTOLA VALLEY, Calif., July 10, 2025—Bay Area Lyme Foundation, a leading sponsor of Lyme disease research in the US, announced the publication of new research in Frontiers in Medicine based on data from Bay Area Lyme Foundation’s Lyme Disease Biobank. This large-scale study conducted over 10 years at sites on the East Coast and the Upper Midwest demonstrates the need for improved diagnostics and increased follow-up by medical professionals for Lyme disease patients.
Only one-fifth of study participants (23%), enrolled with signs and symptoms of early Lyme, were positive by the CDC’s standard two-tiered test for Lyme disease, which supports previous research that found that it misses up to 70% of cases of early-stage Lyme disease. Further, approximately 1 in 5 patients reported ongoing symptoms at 3 months, including joint pain, fatigue, and muscle pain yet only one-third (35%) of these participants followed up with their healthcare providers about these ongoing symptoms. Due to difficulties in diagnosing Lyme disease and resulting treatment delays, as many as two million people may suffer from persistent Lyme disease, which can be debilitating.
Accurate, timely detection of Lyme disease is critical to preventing long-term complications. Moreover, follow-up from medical professionals with all patients after they complete antibiotic treatment could improve outcomes and reduce the burden of Lyme disease,” said lead author Liz Horn, PhD, MBI, Principal Investigator of Lyme Disease Biobank, a Bay Area Lyme Foundation program which helps to accelerate research by collecting, storing and providing much-needed human biological samples for use in research. “Our data also confirm the limitations of serology testing in early Lyme disease and after antibiotic treatment.”


 Dana Parish
Dana Parish
 Our Ticktective host, Dana Parish, interviews Dr. Neil Nathan, renowned physician and best-selling author. Dr. Nathan specializes in treating chronic illnesses, particularly those related to environmental toxins, vector-borne infections, and complex systemic disorders. With decades of experience in clinical practice, he focuses on understanding the impact of toxins on health and is dedicated to helping patients recover from illnesses that conventional medicine often struggles to address. His bestselling book,
Our Ticktective host, Dana Parish, interviews Dr. Neil Nathan, renowned physician and best-selling author. Dr. Nathan specializes in treating chronic illnesses, particularly those related to environmental toxins, vector-borne infections, and complex systemic disorders. With decades of experience in clinical practice, he focuses on understanding the impact of toxins on health and is dedicated to helping patients recover from illnesses that conventional medicine often struggles to address. His bestselling book, 


 Charlotte Mao:
Charlotte Mao: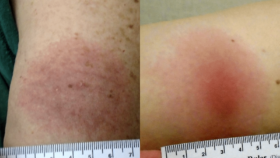
 Anna Schotthoefer, PhD, a project scientist at Marshfield Clinic Research Institute in Wisconsin, discusses the collection and analysis of a specific subset of blood and urine samples for Lyme Disease Biobank—a Bay Area Lyme Foundation program—from patients diagnosed with tick-borne diseases in the state. Marshfield Clinic serves a large population in Wisconsin and Michigan’s Upper Peninsula, which are highly endemic for Lyme disease. Her Bay Area Lyme-funded
Anna Schotthoefer, PhD, a project scientist at Marshfield Clinic Research Institute in Wisconsin, discusses the collection and analysis of a specific subset of blood and urine samples for Lyme Disease Biobank—a Bay Area Lyme Foundation program—from patients diagnosed with tick-borne diseases in the state. Marshfield Clinic serves a large population in Wisconsin and Michigan’s Upper Peninsula, which are highly endemic for Lyme disease. Her Bay Area Lyme-funded 



 Dana Parish: I am so excited today because I’m here with Dr. Todd Maderis. Thank you so much for being here today. I’m thrilled to talk to you. Let me tell you a little about Dr. Maderis. He’s the founder and medical director of
Dana Parish: I am so excited today because I’m here with Dr. Todd Maderis. Thank you so much for being here today. I’m thrilled to talk to you. Let me tell you a little about Dr. Maderis. He’s the founder and medical director of