FOR IMMEDIATE RELEASE
New Bay Area Lyme Foundation Study Reports That Only One-Third of Early Lyme Patients with On-Going Symptoms Followed up with their Healthcare Providers
The new research, published in Frontiers in Medicine, points to need for greater follow-up from medical professionals to address potential treatment failures.
PORTOLA VALLEY, Calif., July 10, 2025—Bay Area Lyme Foundation, a leading sponsor of Lyme disease research in the US, announced the publication of new research in Frontiers in Medicine based on data from Bay Area Lyme Foundation’s Lyme Disease Biobank. This large-scale study conducted over 10 years at sites on the East Coast and the Upper Midwest demonstrates the need for improved diagnostics and increased follow-up by medical professionals for Lyme disease patients.
Only one-fifth of study participants (23%), enrolled with signs and symptoms of early Lyme, were positive by the CDC’s standard two-tiered test for Lyme disease, which supports previous research that found that it misses up to 70% of cases of early-stage Lyme disease. Further, approximately 1 in 5 patients reported ongoing symptoms at 3 months, including joint pain, fatigue, and muscle pain yet only one-third (35%) of these participants followed up with their healthcare providers about these ongoing symptoms. Due to difficulties in diagnosing Lyme disease and resulting treatment delays, as many as two million people may suffer from persistent Lyme disease, which can be debilitating.
Accurate, timely detection of Lyme disease is critical to preventing long-term complications. Moreover, follow-up from medical professionals with all patients after they complete antibiotic treatment could improve outcomes and reduce the burden of Lyme disease,” said lead author Liz Horn, PhD, MBI, Principal Investigator of Lyme Disease Biobank, a Bay Area Lyme Foundation program which helps to accelerate research by collecting, storing and providing much-needed human biological samples for use in research. “Our data also confirm the limitations of serology testing in early Lyme disease and after antibiotic treatment.”







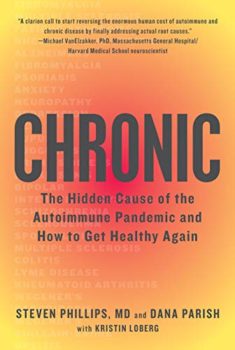 Ticktective host, Dana Parish, talks with her longtime collaborator and co-author of
Ticktective host, Dana Parish, talks with her longtime collaborator and co-author of 

