Below, you’ll find the facts about Lyme disease and the information you need to know.
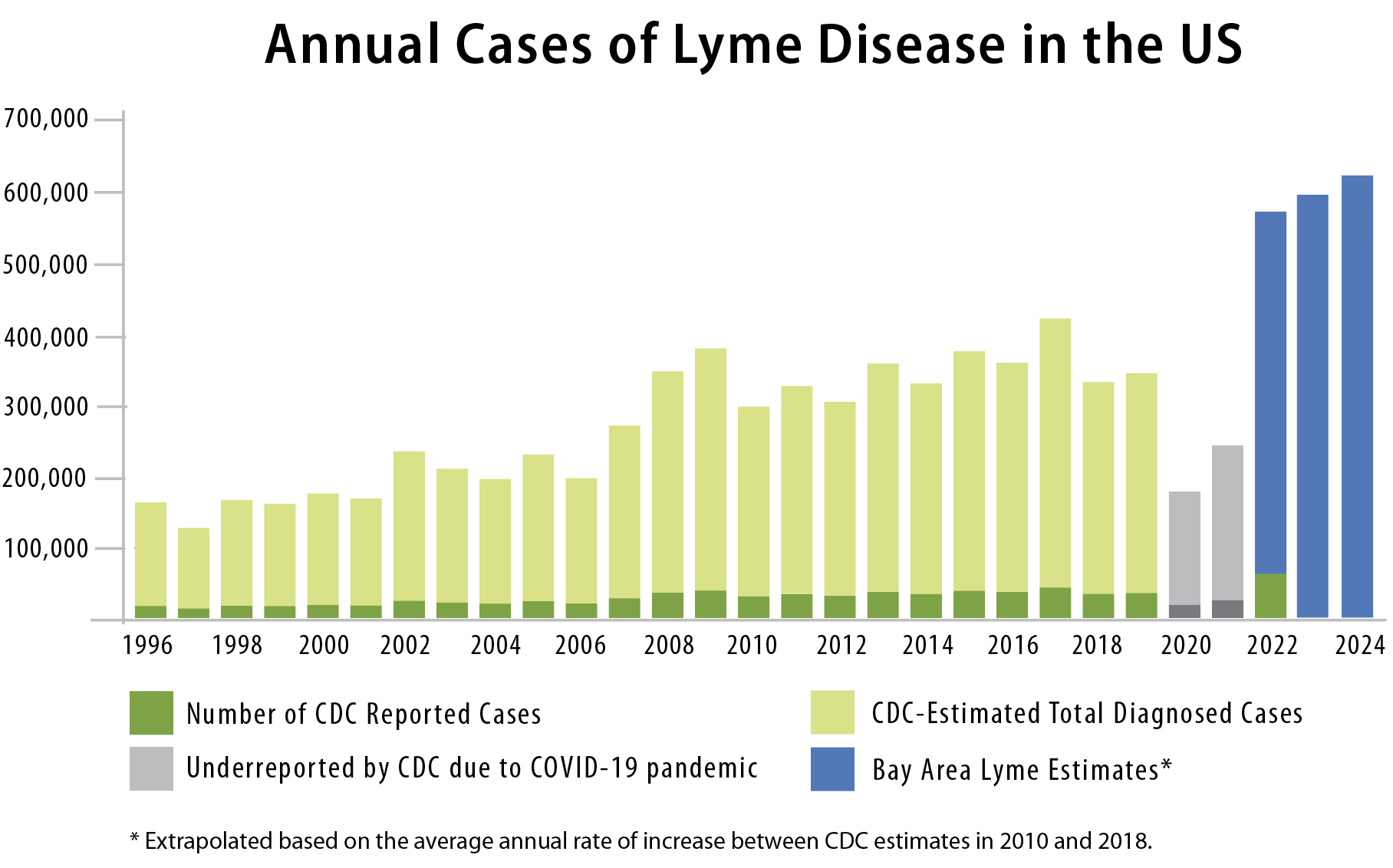
Bay Area Lyme Foundation estimates 620,000+ people are diagnosed with Lyme disease annually
The CDC has long recognized that the number of cases of Lyme disease reported to CDC is significantly less than the actual number of cases. In fact, the CDC acknowledges that under-reporting and misclassification are features common to all surveillance and reporting systems for reportable diseases. The reason for the difference between ‘reported cases’ and ‘estimated actual cases’ of Lyme disease is that there are many requirements for reporting, which, in some states, require the medical provider to interact with the state’s Department of Health.
In 2022, the CDC changed the process for reporting Lyme disease cases. This reporting change increased the number of actual cases reported through this system to over 63,000. This is a significant jump over the reported cases in previous years, yet it is still demonstrably lower than the actual number of cases.
As background, in 2013, the CDC reported there are likely ten times as many actual cases of Lyme disease, based on a survey of seven national laboratories, a national patient survey, and insurance claims data. The CDC also analyzed insurance claims data from 2010–2018 to estimate that 476,000 people may have been diagnosed and treated for Lyme disease in 2018, with the estimated cases rising an average of 5% each year between 2010 and 2018. Based on this average annual rate of increase, Bay Area Lyme now estimates that there were 572,543 actual cases of Lyme disease in 2022.
Using the same 5% growth rate imputed by the 2010-2018 increase, we estimate there will be approximately 627,927 actual Lyme disease cases in 2024.
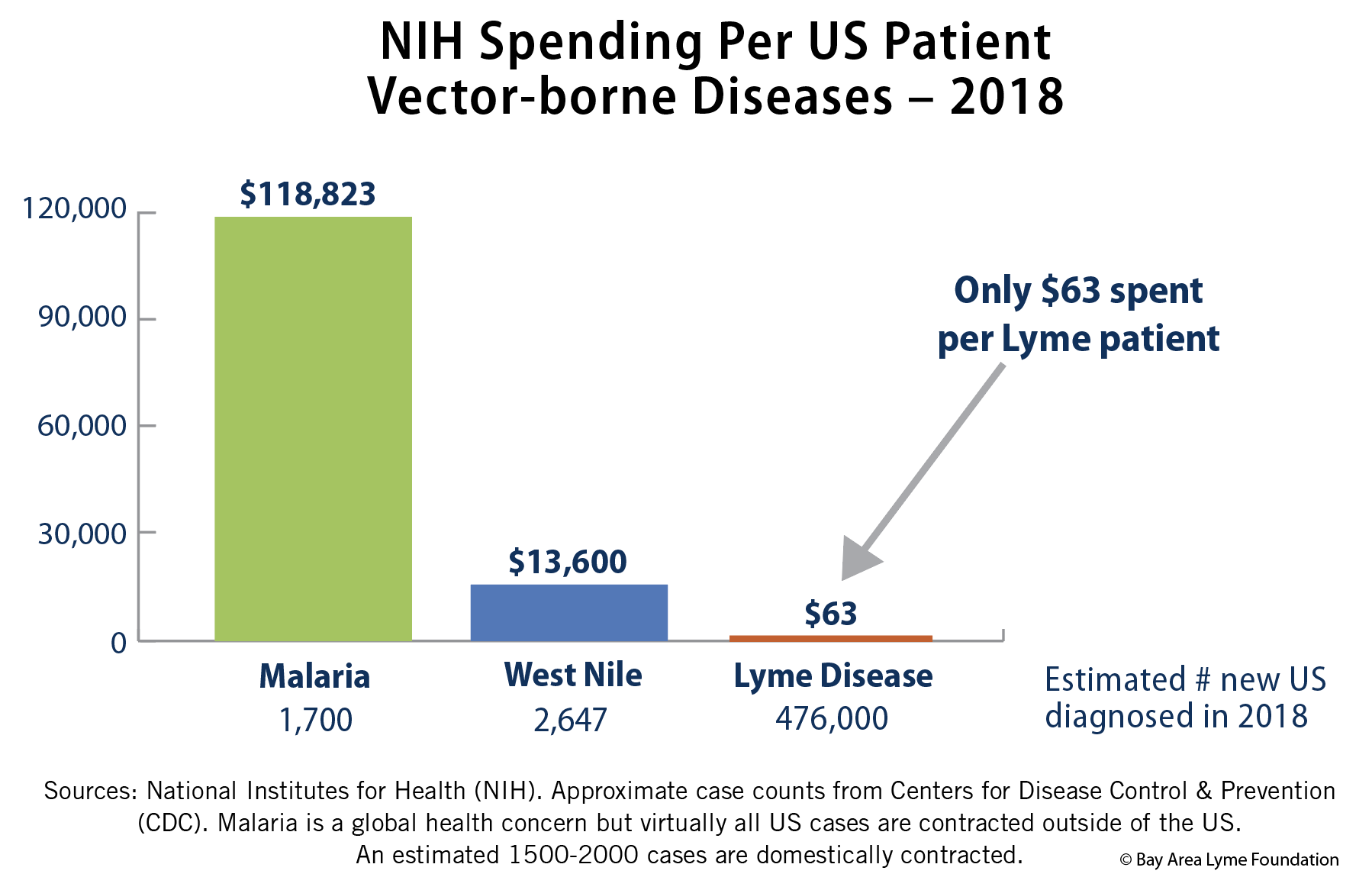
Public funding is far below that of less common illnesses
Lyme disease is one of the fastest-growing infectious diseases in the country and yet Lyme research is dramatically underfunded. It receives less than 2% of public funding for West Nile and 0.2% of funding for HIV/AIDS, despite the fact that the annual case count for Lyme dwarfs either disease. In 2018 there were almost half a million new cases of Lyme disease annually in the US—this is more than the number of US cases of HIV/Aids, West Nile virus, and Malaria combined.
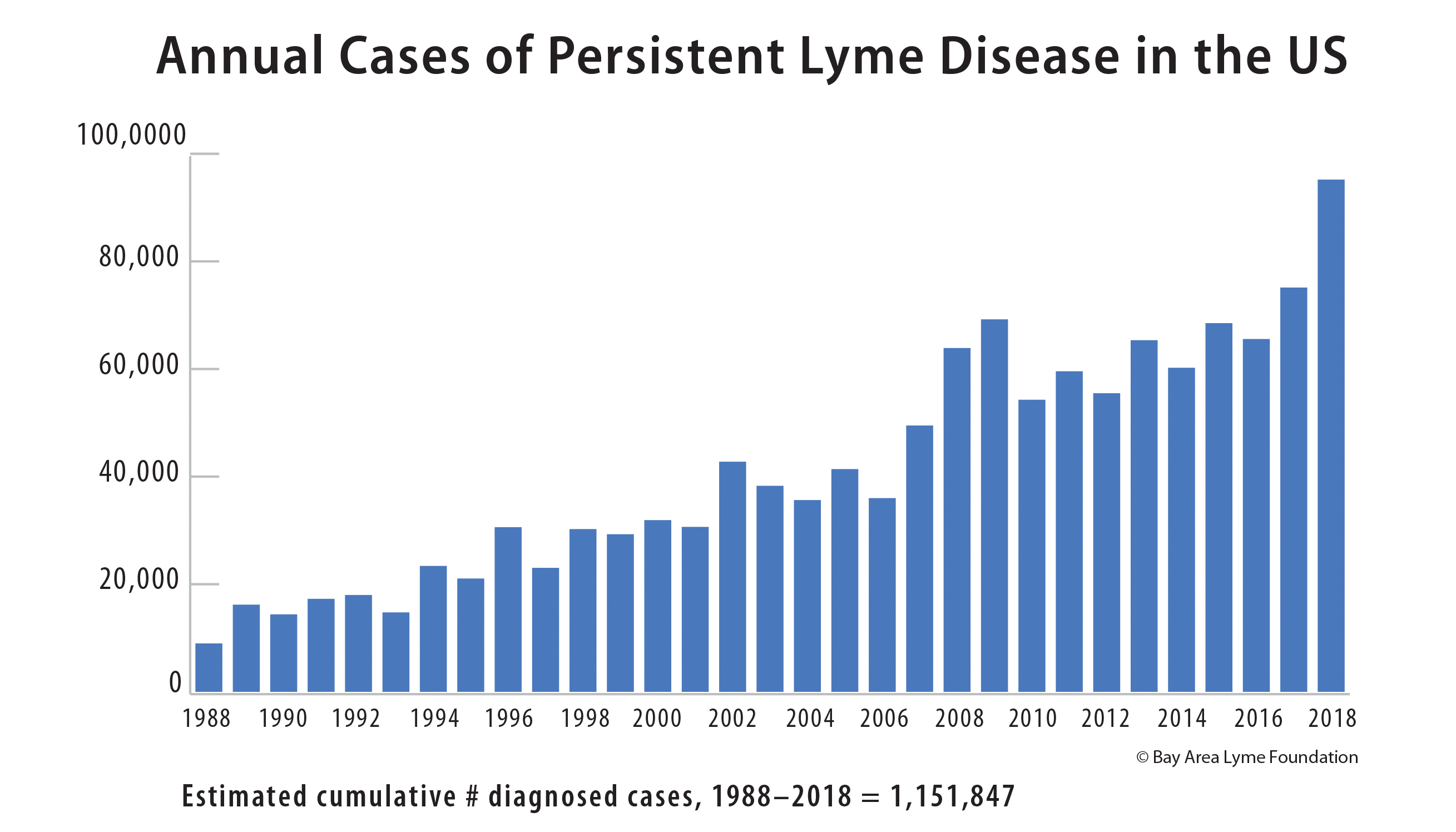
Up to 2 million patients struggling with persistent Lyme disease
Research has shown that up to 34% of Lyme patients have symptoms post-treatment. Many clinicians and scientists believe that the persistence of bacteria is a cause of these lingering symptoms, so, while the CDC calls this “post-treatment Lyme disease syndrome,” many experts believe it is more accurate to use the term “persistent Lyme disease.” These studies demonstrate the existence of persistent infection, giving validity to this term.
Reported in all 50 US states and more than 65 countries worldwide
The disease which was first discovered in New England (Lyme, CT) has been expanding its footprint across the continent with cases as far east as South Dakota and as far south as Florida. Lyme disease was first discovered in California in 1978, not long after it was found on the East Coast.
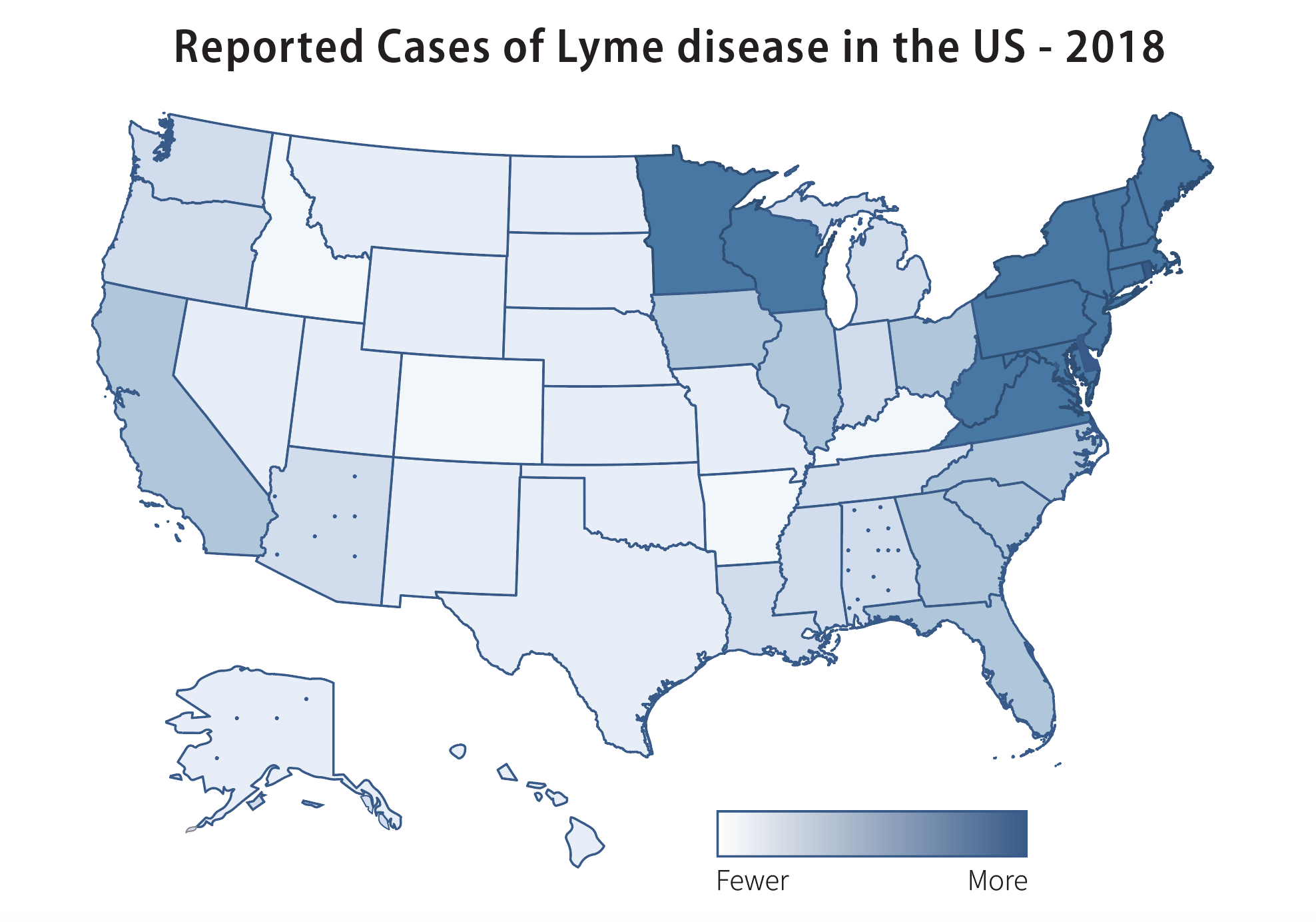
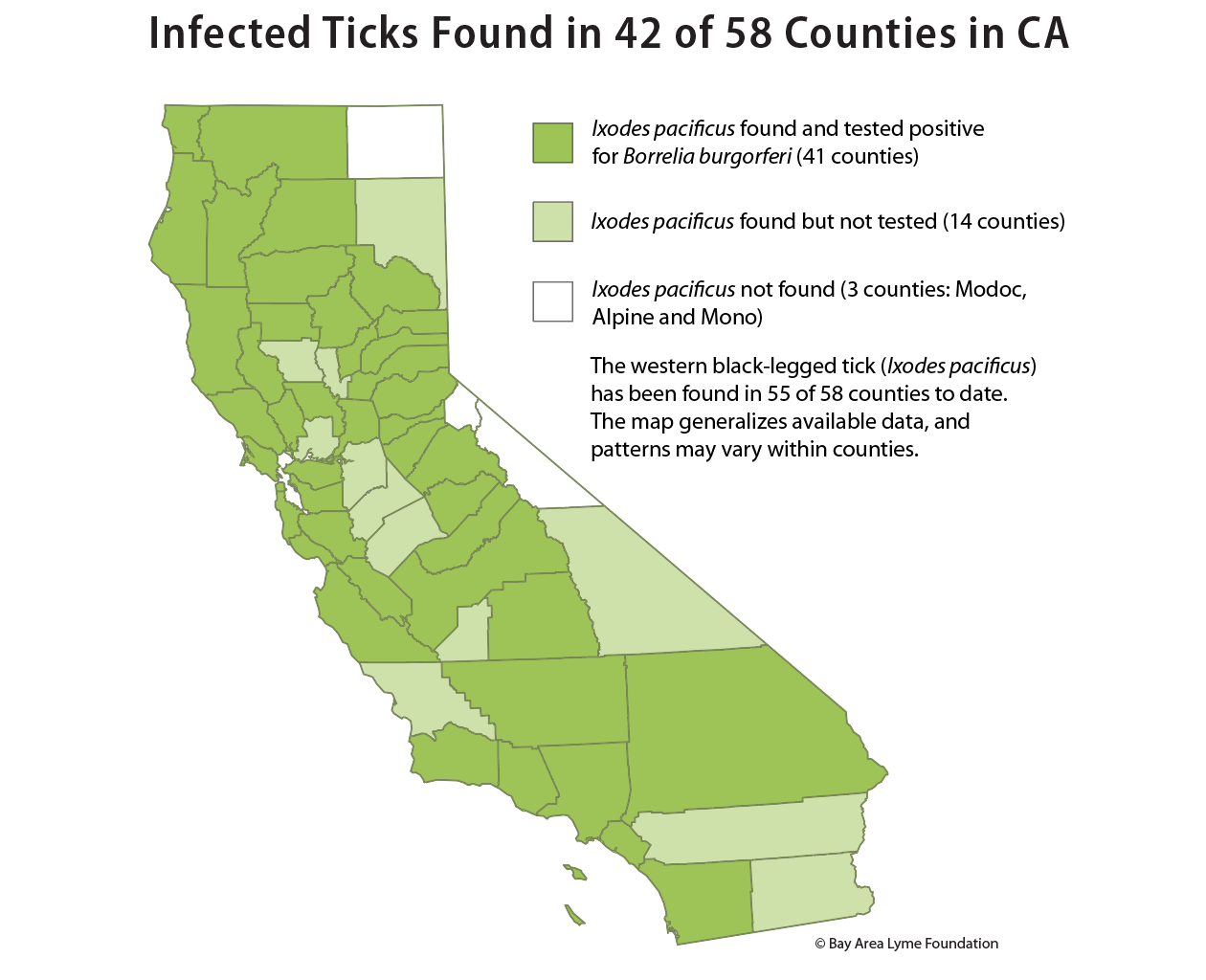
In California, infected ticks were found in 42 of 58 counties
On the West Coast, the primary carrier is the Western blacklegged tick, or Ixodes pacificus, and its principal host the grey squirrel. (This differs from the East Coast where the Eastern Blacklegged tick, Ixodes scapularis, is the principal carrier and the white-footed mouse its primary host.). The Western blacklegged tick has been found in all but two California counties (56 in total) and ticks infected with Borrelia burgdorferi have been discovered in 42 counties.
Current diagnostics miss up to 60% of acute cases
The current “gold standard” diagnostic for Lyme disease is a either a two-tiered ELISA/Western Blot blood test, or a modified two-tiered test of two ELISA testsmeasuring human antibodies against Borrelia burgdorferi. This diagnostic is an indirect measure of infection, detecting the body’s immunologic response to infection rather than detecting the Lyme bacteria itself. It misses up to 60% of cases of early-stage Lyme disease, as it can take weeks for the body to develop measurable antibodies against the infection even if the erythema migrans rash is present.
Early treatment is typically successful but many patients go undiagnosed for years
- Most never recall being bitten
- Less than one-third ever show the telltale bullseye rash, which is an atypical presentation of erythema migrans
- As many as 34% continue to experience symptoms even after treatment
Click here to download our FAST FACTS flyer.