BAL Leading the Way Series
“My family knows that after I die, my tissues will be donated to Lyme Disease Biobank to provide researchers with the vital material they need to solve this horrible disease. I urge anyone with chronic/persistent Lyme to register with NDRI today. Let’s end this suffering together.”
-Kirsten Stein, Lyme Advocate
Lyme Disease Biobank®, led by Liz Horn, PhD, MBI, is central to Bay Area Lyme Foundation’s 10-year search for answers to Lyme’s most intractable questions and is the most important program in the Foundation’s mission to make Lyme disease easy to diagnose and simple to cure.
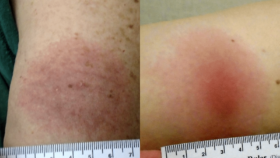
The original Lyme Disease Biobank sample collection launched in 2014 focused on obtaining blood, urine, and serum samples from patients with early/acute Lyme disease. Once this program had been fully established, the Lyme Disease Biobank team explored adding tissue samples to the Biobank. Tissue samples could help researchers expand their investigations beyond the early stage of infection into how chronic/persistent Lyme and other tick-borne diseases impact the central nervous system, joints, and organs of Lyme patients.
With the tissue bank objectives defined, the Biobank connected with specialist organizations to provide the critical support needed to support sample collection and make the development of a tissue bank a reality.
Post-Mortem Tissue Collection Planning
 Lyme Disease Biobank established a key partnership with the nonprofit National Disease Research Interchange (NDRI) to provide logistics for post-mortem tissue collection for the new tissue program. The Biobank also partnered with MyLymeData.org, allowing Lyme patients registered with the Biobank to link their MyLymeData profile to their tissue donation if desired. Bringing these two resources together provides for the organizing and recovery of post-mortem (after death) tissue. It ensures samples include redacted (removes identifying information) detailed patient medical histories—an important nuance for Lyme disease researchers.
Lyme Disease Biobank established a key partnership with the nonprofit National Disease Research Interchange (NDRI) to provide logistics for post-mortem tissue collection for the new tissue program. The Biobank also partnered with MyLymeData.org, allowing Lyme patients registered with the Biobank to link their MyLymeData profile to their tissue donation if desired. Bringing these two resources together provides for the organizing and recovery of post-mortem (after death) tissue. It ensures samples include redacted (removes identifying information) detailed patient medical histories—an important nuance for Lyme disease researchers.
 “Although it is an emotional and difficult idea for anyone to plan to donate parts of their body to science after they have died, we believe that this decision is an important way for Lyme patients to change the course of Lyme disease research. Having access to tissues from the brain, heart, joints, and central nervous system of Lyme patients allows researchers to prove unequivocally that Lyme is present in tissue and contributes to patient suffering,” explains Linda Giampa, Executive Director, Bay Area Lyme Foundation and board member of Lyme Disease Biobank.
“Although it is an emotional and difficult idea for anyone to plan to donate parts of their body to science after they have died, we believe that this decision is an important way for Lyme patients to change the course of Lyme disease research. Having access to tissues from the brain, heart, joints, and central nervous system of Lyme patients allows researchers to prove unequivocally that Lyme is present in tissue and contributes to patient suffering,” explains Linda Giampa, Executive Director, Bay Area Lyme Foundation and board member of Lyme Disease Biobank.

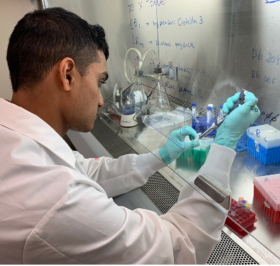
 Anna Schotthoefer, PhD, a project scientist at Marshfield Clinic Research Institute in Wisconsin, discusses the collection and analysis of a specific subset of blood and urine samples for Lyme Disease Biobank—a Bay Area Lyme Foundation program—from patients diagnosed with tick-borne diseases in the state. Marshfield Clinic serves a large population in Wisconsin and Michigan’s Upper Peninsula, which are highly endemic for Lyme disease. Her Bay Area Lyme-funded
Anna Schotthoefer, PhD, a project scientist at Marshfield Clinic Research Institute in Wisconsin, discusses the collection and analysis of a specific subset of blood and urine samples for Lyme Disease Biobank—a Bay Area Lyme Foundation program—from patients diagnosed with tick-borne diseases in the state. Marshfield Clinic serves a large population in Wisconsin and Michigan’s Upper Peninsula, which are highly endemic for Lyme disease. Her Bay Area Lyme-funded 
 The
The 
 In this blog, part of our 10-year anniversary blog series, we talk with John Aucott, MD, Associate Professor of Medicine at Johns Hopkins University, Director of the Lyme Disease Research Center, about his work and how his investigations are helping us understand persistent/chronic Lyme infections. A long-term collaborator and grant recipient of Bay Area Lyme Foundation, Dr. Aucott reflects on his history with our organization, the ongoing plight of Lyme disease patients, and the slow growth in government funding for investigations into the disease. He talks about the early days of identifying the need for well-characterized samples from Lyme patients and his role in helping launch biobank programs, including his own SLICE Study Biorepository and BAL’s Lyme Disease Biobank.
In this blog, part of our 10-year anniversary blog series, we talk with John Aucott, MD, Associate Professor of Medicine at Johns Hopkins University, Director of the Lyme Disease Research Center, about his work and how his investigations are helping us understand persistent/chronic Lyme infections. A long-term collaborator and grant recipient of Bay Area Lyme Foundation, Dr. Aucott reflects on his history with our organization, the ongoing plight of Lyme disease patients, and the slow growth in government funding for investigations into the disease. He talks about the early days of identifying the need for well-characterized samples from Lyme patients and his role in helping launch biobank programs, including his own SLICE Study Biorepository and BAL’s Lyme Disease Biobank.