– Bonnie Crater, founder and vice-chair of the Board of Directors, Bay Area Lyme Foundation
“I was driving down a road that I’ve driven 1,000 times and suddenly I had no idea where I was or where I was going. So, I pull over to the side of the road to get myself oriented, and then 5-10 minutes later, I remembered and drove to my destination.”
Several friends affected by Lyme have told me of this same experience. It’s caused by the brain fog symptom of Lyme disease, which is often called “mild cognitive impairment” by physicians. I first learned about brain fog when my friend Laure and I founded the Bay Area Lyme Foundation. She explains it like this:
“My nature is to be prompt, attentive and on top of things. It’s important to me to remember people and conversations, and follow up later. Brain fog makes me feel like my brain is muffled with cotton, and it turns me into a “flake” which is very frustrating and hard for me to accept. There are times my brain has been so confused and my spatial awareness is so poor that I’ve actually walked right into a wall. Often, when I am experiencing brain fog, I have to read paragraphs numerous times, and can’t comprehend the content or remember the beginning of the paragraph by the time I’ve gotten to the end.”
As you can imagine, experiencing brain fog—and the cognitive dysfunction involving memory problems, lack of mental clarity, and poor concentration that comes along with it—is very scary for Lyme patients.
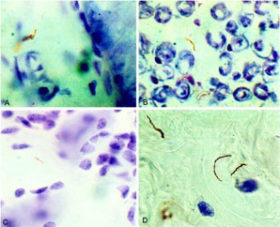
So, what is brain fog? It is defined as a temporary state of diminished mental capacity marked by inability to concentrate or to think or reason clearly. For Lyme patients, brain fog seems to manifest by decreasing your ability to think, causing you to feel confused or disorganized and making it difficult to focus or put thoughts into words. So, why do Lyme patients suffer from it? To unpack this a bit, let’s look at some research. Nearly 20 years ago in 2000, Dr. Diego Cadavid and other researchers published a study in Nature where they explored the dissemination of the Lyme bacteria Borrelia burgdorferi (Bb) in non-human primates. They found the bacteria in several organs including the skeletal muscle, heart (aorta), and bladder. They also found the bacteria in the primate brains (pictured below).
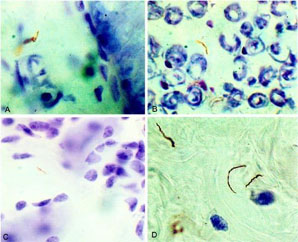
For some Lyme patients, the brain fog they experience can, in severe cases, resemble some phases of Alzheimer’s disease. In a curious related finding, Dr. Alan MacDonald discovered Bb in a large percentage of Alzheimer’s brains—7 of 10 Alzheimer’s brains had signs of a Bb infection in his 2007 pilot study. If Bb and brain fog are connected, that raises an interesting question: How might infection with Bb in the brain be causing brain fog?
In 2012 I met Jay Rajadas at Stanford University. His father-in-law sadly had Alzheimer’s disease, and Dr. Rajadas became very interested in studying amyloid plaques found in the brain of Alzheimer’s patients. He also wanted to investigate a possible connection to Borrelia infection. To gain more insight, Dr. Rajadas initiated a study and Bay Area Lyme Foundation and the L.K. Whittier Foundation funded this initial research. By 2015, Dr. Rajadas had started collaborating with additional researchers. Together, they conducted laboratory and mouse studies to understand the impact Bb may have on neurons in the brain. They hypothesized that the lipopeptides, fatty compounds that are sloughed off by the Bb bacteria, may interfere in the communication between neurons. They conducted PET scans on mice and tested the effect of the presence of a synthetic lipopeptide on the communication of neurons. What they found is that, in the presence of the lipopeptide, the density of the communication sites between neurons were significantly lower and there was a disruption in the synaptic signaling. This result suggests that some neural pathways might get disrupted. Could this disrupted signaling be causing the brain fog?.
What does this mean for Lyme patients? This week, results of years of hard work were published in the Journal of Neuroscience that provide clues that answer this question. For the first time, researchers have demonstrated that lipopeptides associated with Bb cause dysfunction in the brain of mice. It also gives us more to consider.
If this research is confirmed by others, we now have a new hypothesis to test: Do lipopeptides disrupt neural pathways? And, if we can keep Lyme patients free of lipopeptides in the brain, will they stop having brain fog symptoms? While the lipopeptide effect is exciting new information, more research is needed to confirm these findings and find solutions for Lyme patients. The work today offers another clue about how Lyme disease causes neurological symptoms and another piece of information we can use to solve the Lyme disease problem.
Our hope is that one day Lyme disease will be easy to diagnose and simple to cure.
I don’t thik that the comment above, that Rocky Mountain Spotted Fever is Lyme disease, is correct. Doctors I have worked with do not consider that to be correct.
I was diagnosed with Rocky Mountain Spotted Fever almost 20 years ago. In the last 5 years, I’ve started forgetting things — such as memories of my childhood in the beginning and then it got to where I would forget things from minutes ago. I told my PCP about the issues I was having and was referred to a psychologist who diagnosed me with ADD. The meds seem to work for a few days but then it is like I become immune to them. I still have very few memories of more than 3 years ago. Does anyone have any essential oil treatments that may help with these issues? There are no local doctors to help with what I believe the issue to be.
I was diagnosed with infection from Borrelia, Babesia, and Bartonella about a year ago. I was forgetting things as well as having chronic brain fog, terrible pain in my knees, and bodily fatigue, etc. My doctor has put me on Disulfiram (Antibuse) which is an antibiotic originally given to alcoholics, and it makes you sick if you consume alcohol when on it. Long story short, it has been discovered to treat all of these bugs simultaneously, while the botanicals I was taking only treats them one at a time, and not as effectively. I am still on the road to recovery, but I seem to be getting better slowly but surely, and hope to be cured soon, as my dream has been to become a Navy SEAL. My doctor believes that it is never too late to treat Lyme with antibiotics, provided they are appropriate for your case. Additionally, dieting has been a huge help for me, as eating lots of sugar and dairy make my brain fog terribly worse. Screen time also seems to increase my brain fog and eye strain, so I’ve cut that down by a lot as well. I also recently purchased a PEMF Regenitron machine and red light machine(both of which my doctor is also a huge believer in), and using the PEMF for just 30 minutes a day and the red light for 15 minutes a day makes a world of difference long term. They are a bit expensive, but totally worth it, and you get what you pay for! I hope this was a help to some of you, desperate for options, just as I was. I will be praying for God to help get you through this, as he is doing for me now. God bless!
Rocky Mountain spotted fever is Lyme disease. Find a good Lyme literate Dr ASAP. If you where never treated then you still need medical treatment for Lyme disease.
Rocky Mountain Spotted Fever [RMSF] is actually not Lyme, though it is potentially very serious bacterial disease and many of its symptoms are similar to those of Lyme. Importantly, RMSF is contracted by a bite from a dog tick, not a deer tick (as is Lyme). (The dog ticks are typically larger and easier to spot.) Most Lyme-literate care providers are knowledgeable about other tick-borne illnesses and can indeed help you.
Lions mane mushrooms helped me. I still suffer forgetting where i place things daily but this supplement has helped me not feel so hopeless like i have full blown dementia.
“I was driving down a road that I’ve driven 1,000 times and suddenly I had no idea where I was or where I was going. So, I pull over to the side of the road to get myself oriented, and then 5-10 minutes later, I remembered and drove to my destination.”
This is exactly what happened to me. Exact same situation in the car, all of a sudden I did not know where I was or where I am going, reacted the same way and pulled over. It is kind of a temporary amnesia, which is extremely scary.
I can’t believe what I’m reading..it’s me to a t. This is the worst depression, scary, etc. How do we just forget how to get home, or who we are or etc.? … This has been me a lot lately. I’ve often said I have Alzheimer’s. Reading this article makes me think the very being of Alzheimer’s is because of a tick bite. I’ve never been so sick in my life. I can’t eat dairy, red meat, etc. I have found myself trying to figure out how to get home sitting trying to map where I am..😢. Praying for everyone.
If Lyme bacteria Borrelia burgdorferi (Bb) is the root cause for Lyme disease, then perhaps the natural products obtained from the herbs can be tested in-vitro and if the potency of any one or combination of more than one compound is proved, then it may not be that difficult to prove in in vivo studies and also in clinical studies. I think, jay work has laid foundation for further studies in this direction.
Samento and banderol combo from Nutramedix has shown to be effective in treating all the forms of Lyme from spirochete to cyst:
https://www.townsendletter.com/July2010/sapi0710.html
Blessings:)
oops – forgot to put in the name of the herbal parasite cleanser – Purify. It works really well. Just wondering if it sent the parasites elsewhere.
Lyme – 3 yrs ago. The brain fog, which subsided during the first year of treatment, has increased suddenly after a few months of treating intestinal parasites with something called _ that contains a lot of clove. And when I am anxious it increases instantly. Also, after drinking black tea or coffee, not nearly as much with green tea. It feels like something is expanding inside my whole head and I can’t think. It had been subsiding with Glutathione and lots of water. Now that doesn’t work. So scary.
Please get on IlADS for doctors to travel to — sign up to get info it’s free. Google LLMD, integrative medicine, get an ND or herbalist that treats. Test for EBV and Lyme. Most insurance covers, even Medicare. Get additional financing care credit, greensky, denefits. Get in FB groups, try low-dose naltrexone, Low-dose immunologytherapy, Des bio homeopathic borrelia/ basbesia, dapsone protocol, biofilm Buster’s, raw eggs with shells or amino acids and green drinks. No regular doctor will help u. Save up to 500 to 1, 000 to get started. Help is out there. U gotta find it. Chiropractors who are LL Lyme literate and do functional medicine will help u. Some start at 300, get testing done at right labs or specialty. I went to Cleveland clinic for gut, then Michigan to integrative and blood work done at St. Joseph mercy for specialty testing. Pray about it and it can be done.
Are you better now?
My granddaughter was dx with Lyme, Reading all research I can find. ty.
As ridiculous as it may sound, I strongly recommend to get a vaporiser and try a couple of drops of Clove Oil. Just leaving this in my immediate vicinity for 6-8 hours over 2 days caused quite a severe Herxheimer reaction from the die off, that lasted 72 hours. Especially try this if you have a dermal fungal/biofilm infection. It cleared mine up in just a few days. I’d had this for 5 years apart from a 10-month period after taking 3 courses of Ivermectin. I never experienced a die-off at all from the Ivermectin. I’m pretty sure that taking a drop or two of clove oil internally will be even more potent.
My daughter just got diagnosed with Lyme dz. I’m starting to think she has had it for a while, and not just recent. She was already having the brain fog, headaches, joint aches, vertigo, etc., extreme exhaustion… Does this sound like a recent infection or that she has had this for a while? She is still on her 30-day course of antibiotics, and at the end I am asking her pediatrician to send her to a specialist. I am worried for long term effects and she is 17 and in my part of Texas, not much is not known about Lyme. I had to ask for her to be tested only bc of the remembrance of my little brother having it as a teen when we lived on the east coast and sure enough, she was positive on her lab tests. Looking for any kind of information they I can!
I’ve been taking antibiotics and other medicines for a year and a half now to treat two diseases from tick bites that went undiagnosed for 7 years (that is the estimate because that is when the symptoms started). The longer it is undiagnosed, the longer you should take the medicines for it. There are 9 in all that affect humans. Lyme is the most common, but the second most common is 50% as common as Lyme and just as bad. Go to a tick disease specialist to be tested for these other diseases and get the best treatment. General physicians are taught very little about these diseases in med school and will not be able to help much.
Sounds like long term Lyme, like I’ve had. I took three types of antibiotics for 11 months. I just couldn’t take one more pill. I’m much better off, but still not the same as I was. Be patient. Be kind. Lyme very much makes a person feel isolated.
God bless you.
I’m asking Patrick Jordan about Hulda Clark Zapper. Did you ever experience Lyme healing with this method? Also, did you hear about the Andersen family and their lyme success story? Obtained with diet only?
I was misdiagnosed with early-onset Alzheimer’s back in 2007 using a CAT scan designed to detect brain cancer (glucose uptake). My symptoms were similar to the article, except for the emergence of 50-year-old memories as is commonly found in Alzheimer’s patents. My neurologist would not accept my suggestion of neuroborreliosis and forced me to retire with a disability. My symptoms continued to improve and, in 2017, I was retested with a new amyloid PET scan and found amyloid-free. Neuropsychology testing showed a 95% recovery. I don’t know if ten years of Razadyne and Namenda helped.
Congratulations to Jay Rajadas and his team for their interesting research studies and results. Wish him and his team further success in their ongoing investigation.
I’m not sure if I have Lyme or not. Just got a blood test done. I have bad anxiety and panic attacks. I feel like I can’t breathe normally, like I use to heart populations, my finger joints are swollen, blue veins all through my fingers and hands, and my legs hurt walking up the stairs. I have like no energy anymore. I’m always so sleepy as well. I just recently started getting headaches and back pain now also my head feels stuck in like a blur and won’t go away. It’s been 7 months now and it’s been awful. Also shooting pains going up my arms too…
Good that you getting tested. You should try to be diligent about documenting all symptoms — when, what, how severe, how long, if changes, etc. — and even take photos of any rashes or lesions, etc. It will help your doctor diagnose. Also, if you were bitten and/or suspect a tick or other insect bite, also helpful to note any details about when and where you might have been infected will be helpful. Best wishes for a fast diagnosis and treatment.
If you did the basic ELISA, I wouldn’t count on it being accurate. It sounds like you have co-infections too. When I went to listen to a lecture by Dr. Horowitz, he said coinfections are a rule, not an exception.
Babesia can cause air hunger and panic attacks. Bartonella causes many neuro issues and panic attacks too. Both are hard to treat and diagnose as well. Like Lyme, they both have a multitude of possible symptoms and present differently in everyone. Try to find a good LLMD or LLND to help you. There are also other infections you could have and you need someone who doesn’t solely rely on labs. You need someone who can clinically diagnose as well. Hope this helps!
My name is bob.tree cutter 35 years.some days want to break down and end it.pulled 20 ticks off me past summer.i don’t like to talk about symptoms.u think I’m crazy.mind feels shot confused eye focus change
Lyme brain fog could most easily be explained by circulating pro-inflammatory cytokines, which is likely why it clears when people take stimulants. Stimulants decrease pro-inflammatory cytokines and also help decrease pain due to Lyme disease.
What stimulants?
More importantly: WHAT pro-inflammatory cytokines? The immune signalling chemicals are not the enemy. As Alan MacDonald showed, it is the filarial worms burrowing into the CNS that bring the Borellia in like a taxi cab that are the problem, so without the inflammation there will be no immune response and without an immune response then there will be no addressing the invaders, therefore all that was accomplished is TOLERANCE which will let the invaders create havoc, but the victim will just not feel it. What is the Kill Shot for the worms and spirochetes?
“Lyme brain fog could most easily be explained by circulating pro-inflammatory cytokines, which is likely why it clears when people take stimulants.” Thank you for mentioning this!
I’ve personally experienced a release from Lyme brain fog while taking phentermine for weight loss. After a month I described to my doctor that I felt like I was in the movie Limitless. The difference was incredible. Is there research to back stimulants being beneficial for brain fog? It’d be a lot easier to justify long term use for a diagnosis other than weight loss.
I discovered my bullseye third week of July 2013. There’s a lot to the story. My brain is working just like what you described in this article. I think I have a solution to get the brain’s connections working properly. Please don’t laugh or think I’m nuts. I chewed a very small pinch of magic mushrooms. For three days all the racing, fog and forgetfulness disappeared. There were no hallucinations by the way. Calmness, yes. If this is what normal feels like, I want more. Please contact if you would like hear more.
Nothing to laugh at, but cause for great concern. It is well documented that Lyme & company facilitate viral re-activation or infection. So far, we have identified that opioids and anything that work on those neuroreceptors allow cell permisivity to Herpes virus, at the very least; this implicates alcohol as well. THC allows viral penetration. Next we were to look into nicotinic and muscarinic receptors but there is just so much a few humans can do in a lifetime. Clearing symptoms seems to be the focus in the guru sphere of dealing with Lyme but mostly the interventions only create tolerance for the invader, never getting rid of the root cause. I don’t deny the perception of removal of symptoms, I just question the mechanism of action.
I am interested in hearing more. I’m having a real difficult time with brain function/ rational thinking right now.
My son has brain fog and weakness of body for seven years. We recently found out that he has Lyme. The antibiotics did not help. He is fed up and feels that a psychologist would help but I am trying to get him to take natural herbs etc. Can you elaborate on what you took? Thanks.
I’m a 68-year-old grandpa that’s had seven back surgeries, shoulder repair, and left new knee. Been fighting Lyme disease for nine years. Muscles hurt, joints hurt, brain fogs. The list goes on and on. My entire family has this disease and a buddy of mine and his family. We know where we got it. I pray everyday for my grandchildren and children for some type of relief. I’m getting tired of fighting and surgeries are no longer an option because of my brain and lungs. You reach a point of your life where you say enough is enough. Basically our families are bankrupt. We live day-to-day, paycheck-to-paycheck.
Bill, My son has Lyme disease, but is not sure how he got it. You say that you and your family know where you got it and I would like to pass that information on to my son. Thanks so much, Harry Lee
Bill, both of my children and I have it as well. It’s amazing in the Lyme groups how often you see whole families with Lyme. It’s not talked about enough. Like you, desperate for relief but even more so for my children.
I am an FNP. I have been treated for Lyme for several years. How can I get involved in research?
This blog post may give you some answers about the pros and cons of getting involved in clinical research and some next steps.
I have brain fog…I am a Diabetic..I have had tick bites and now have lots of sores with the center missing. I stay tired. I do my house work if I feel like it. I am 71. I am a Registered Nurse. I have had no luck finding someone to help me. I now have one patient. Me: I itch most of the time. Take a lot of Benadryl. I have wondered if I have Morgellons Disease or Lyme disease. I live in a small town in Kentucky. The doctors don’t have a clue. I do a lot of research on this. I need help. I just asked for an EGD. It was done 3 days ago. I can’t eat. Have heartburn extremely bad and bloating..Not psychotic, this is real. I need help.
Carla, If you suspect Lyme or a tick-borne disease, we would strongly encourage you to see a specialist familiar with these illnesses. The International Lyme and Associated Diseases Society (ILADS) maintains a database of clinicians and can point you in the direction of an informed care provider in your area. Continue to document your symptoms including description; date, time, and duration of incidence; and any changes (improvement or deepening) of symptoms. You may even want to take photos. The more information you can share with your doctor, the better equipped they will be to diagnose. Best wishes.
I am studying the work of a fellow who links Morgellons to the Bartonella co-infection of what is falsely called Lyme. Since tickspit must contain more than just spirochetes, it can never just be spirochetes but polymicrobial infection. MacDonald demonstrated filarial worms as the delivery vehicle for the Borrelia. Those burrow through the body like swiss cheese, so itching would be a given with just the nematodes, let alone all other causes. Why antibiotics are pushed like used car sales but anti-parasite herbs are never mentioned is a crime in itself. Another thing we are trying to harmonize is the totality of spirochetal presence: Leptospirosis is as easily gotten as a kiss from a dog or horse that has been rooting in the dirt. Helicobacter Pylori is yet another pandemic that is covered up worldwide. Hulda Clark said that reflux was from bacterial overgrowth on the hiatus. If the sphincter cannot close due to muscle weakness then the acid will reflux. Acid was never the enemy, in fact, it is supposed to protect us from the invaders. I have been experimenting with cayenne and tabasco peppers with mixed results because unfermented peppers come with lectins and alkaloids that bring their own problems. Ancient herbal tradition was to make the GI tract inhospitable for the invaders. It seems reasonable, but they might pack up and move to different tissue, so we have to have a comprehensive program to kill them, not just relocate them. Antibiotics create Cell Wall Deficient forms so using allopathic drugs makes the problem a thousand times worse than not treating it. These conditions are never ‘in your head’ except for the fact that neuroborreliosis is… in your head…
Carla, you have to find a specialist that deals with Lyme. They are not easy to locate. Regular MDs don’t know how to test for, nor treat it. It takes a special blood test that only a couple of centers I know of can do.
I went to Dr. Salvato in Houston, TX. Dr. Salvato gave me many rounds of antibiotics and rotated them in and out. There were three kinds, and the system of (off and on) rounds of pills lasted about a year.
I have had Lyme all my life, so it took this long to treat. But because I’ve had it so long, my brain has yet to come back to me, it has been 4 years now. I keep trying to find info on anything that helps brain fog and so on.
This makes me wonder also about memory and the effect Lyme has on it. Both short and long term memory seem to be damaged. In people who have been successfully treated that had these symptoms, are the memories regained or are they gone for good? If short term memories are needed to be translated into long-term ones, will there be no long-term memories from that period of time? Isn’t this part of cognition?
Good question. Wondering this myself. Sitting here very frustrated that I can’t remember things from middle school (25 years ago) that my friends can. Short and long term memory is affected. I used to have a memory of an elephant. Also Mercury and/or mold toxicity can also cause this brain fog and memory loss. Big time.
Well, it’s not that black and white, Mark. People with Lyme or some of the other infections tend to have days, or parts of days, where their minds do OK. Maybe not “sharp as a tack,” so to speak, but well enough to recall pretty well and commit new memories as you would expect. Brain fog varies a lot, and is not the same for everyone.
Old memories come and go depending on the day, and on bad days, it can be like everything is a blur. It’s easier to just sit and watch a bad tv show than to try to think.