Ticktective Podcast Transcript
Dr. Adrian Baranchuk, Professor of Medicine at Queen’s University in the Division of Cardiology in Ontario, Canada discusses his screening process for identifying Lyme infections in the heart and how to treat these patients without unnecessary pacemakers. He has published research and spoken on the topic of Lyme carditis at numerous conferences. He is passionate in his efforts to educate doctors on diagnosing Lyme-related AV heart block. Dr. Baranchuk joined Bay Area Lyme Advisor Lia Gaertner to discuss the cardiological manifestations of Lyme disease, Lyme Carditis and specific cases that illustrate his approach.
Lia Gaertner: Welcome to the Ticktective podcast and video series, a program of the Bay Area Lyme Foundation, where our mission is to make Lyme disease easy to diagnose and simple to cure. I’m your host, Lia Gaertner. Lyme disease is the most common vector-borne disease in the USA and is a global issue. This podcast includes interviews with the researchers we fund, as well as other interesting people in the Lyme scientific community. We are a nonprofit foundation based in Silicon Valley. Thanks to a generous grant that covers all of our overhead, 100% of all donations go directly to support research and prevention programs. You can find out more or donate@bayarealyme.org. Thank you for joining the Ticktective video and podcast series, Dr. Baranchuk
Adrian Baranchuk: Thank you very much for having me.
Lia Gaertner: Dr. Baranchuk, a native of Buenos Aires, Argentina, completed his training in internal medicine in cardiology, along with clinical fellowship in cardiac electrophysiology. Dr. Baranchuk is a tenured professor of medicine at Queen’s University in the division of cardiology in Ontario, Canada. He is the editor-in-chief of the Journal of Electrocardiology, as well as a member of numerous editorial boards and a reviewer for several medical journals. Dr. Baranchuk has authored eight books and published more than 700 articles in prestigious international journals, as well as 54 book chapters, and he’s presented more than 270 abstracts around the world. He is the vice president of the International Society of Halter and Non-Invasive Electrocardiology, and the Secretary of the Inter-American Society of Cardiology. He’s also the past president of the International Society of Electrocardiology. He’s been elected as a member of the Electrophysiology Leadership section of the American College of Cardiology, and is the recipient of several teaching awards as well as being voted one of the 10 most influential Hispanics in Canada.
Adrian Baranchuk: Thank you very much for the invitation. I am so pleased to be here with you today.
Lia Gaertner: I’d like to start with a case study published in the Canadian Medical Association Journal (CMAJ). It reads:
“A fatal case of Lyme disease in a previously healthy 37-year-old man illustrates the challenges of diagnosing Lyme disease in the absence of classic symptoms. The patient originally presented to his family doctor with flu-like symptoms, including fever, sore throat, nasal congestion, and migratory joint pain. Several weeks earlier, he had been in contact with ticks but didn’t recall removing one. His physician suspected a viral infection and the patient’s symptoms resolved. However, weeks later, he developed heart palpitations, shortness of breath, and chest discomfort for which he was sent to the emergency department. Lyme disease was suspected as the ECG showed complete heart block. He was admitted to the hospital and started treatment for Lyme carditis. But his condition unfortunately worsened quickly. Clinicians were unable to reverse the course of his illness, and he died. Serology results confirmed Lyme disease and an autopsy showed Lyme carditis.”
So, that is a really sad story, and I know that the CDC has in the past few years come out with more information about fatal cases of Lyme carditis. And I know that there are a lot of cases of Lyme carditis that fortunately are not fatal but are very serious and some that are mild. But nonetheless, it’s an important thing for physicians to be on the lookout for.
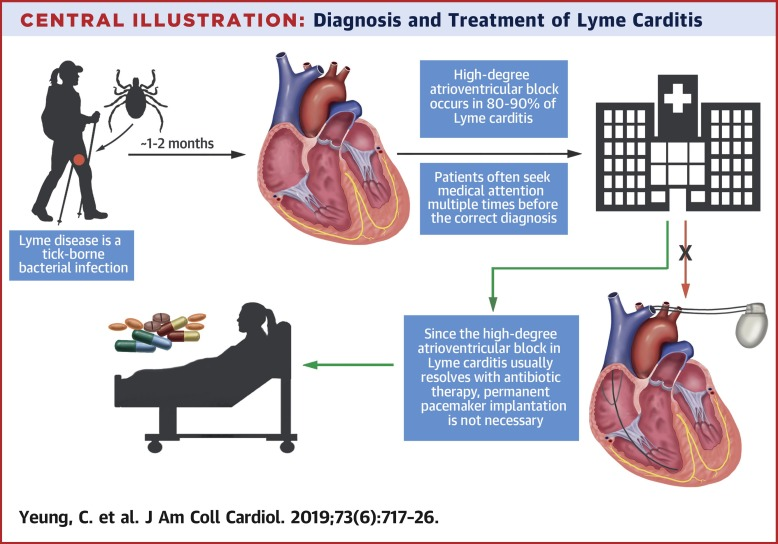
Adrian Baranchuk: First of all, approximately 3-5% of all people presented with Lyme disease may have the cardiovascular system involved in this condition. And it’s more common when Lyme disease is not diagnosed early and treated properly with antibiotics. We call this stage of the disease, “early disseminated Lyme disease,” and one of the organs that can be affected during early disseminated Lyme disease is the heart. When that occurs, we call this Lyme carditis. So, approximately, again, this is in 3-5% of all Lyme disease cases. But if you have 300-400,000 cases of Lyme in the US, just work out the number. It is a significant number of people that will have a heart infection due to Lyme disease.
Now, from the group that develops Lyme carditis, approximately 9 in 10 will present with what we call a “shutdown” of the electrical system. That’s the electricity of the heart that all of a sudden gets interrupted by inflammation of the conduction system, and the heart stops beating.
When this condition is not rapidly recognized it can lead to fatal events as the case that you described. It’s a case that got published recently along with another case from our lab which, thank God, the patient—who is female—recovered nicely, but this helps to illustrate that early recognition and specific action can prevent patients not only having a disabling condition or the need of a pacemaker for the rest of their lives, but also to prevent death. So, this is something that I would like to emphasize: Non-recognized Lyme disease can lead to Lyme carditis, and recognized Lyme carditis can lead to death. This is why a series of researchers in North America are working extensively to educate our peers in the earlier recognition of this condition, because that could help to prevent long-term disability or death.
Lia Gaertner: I know the case that got published in Reader’s Digest based on one of the scientific articles that you put out on the 56-year-old woman. Can you tell us a little bit about that case?
Adrian Baranchuk: This is about a 56-year-old woman. So with that alone, she’s defined as what we call an outlier. Why? Because the predominance of these conditions so far in the literature is about 8 or 9:1 ratio male versus female, and approximately 90% of the people presented with Lyme carditis are younger than 50 years of age. So, a 56-year-old female is what we consider an outlier. She’s outside of the well-known conditions that are associated with Lyme carditis. And this is the first important message of this case, both published scientifically in Canadian Medical Association Journal (CMAJ) and transformed by a fantastic journalist into a more approachable case in the last volume of Reader’s Digest in 2020. This lady presented first to a different hospital with a rash on her shoulder, but not the classic rash that we expect to see in patients with Lyme disease called a “bullseye.” That bullseye rash looks like a target with a red center and then a whitish surrounding area, and then another red area. So, that classic picture we learned does not show in all patients with Lyme disease, and specifically in patients with Lyme carditis it is only present in 30-40% of the cases.
This lady had a quite atypical triangular rash on her left shoulder that was interpreted as cellulitis. The patient went home with some corticoids. She came back a second time and, again, the rash was not clear. Now it was dissipating. She showed the rash on her phone. She explained that she is a runner and she’s fit. Nobody connected the dots. The patient went home with one day of antibiotics. She came back one more time, now feeling dizzy. So, someone said, “Hey, rash and dizziness. Why don’t we do an ECG?”
And in the ECG, unexpectedly, we found what we call a high degree AV block, which is a partial shutdown of the electrical system. So, someone rang a bell and contacted us, and we went to see her immediately. We took serology and we put the patient on cardiac monitoring and IV antibiotics. And from our own experience that got published several times—including a recent paper in the Journal of the American College of Cardiology (JACC) which is a very high impact factor journal—patients can deteriorate very rapidly. But with IV antibiotics, if they have Lyme carditis, they usually improve very quickly. So, this lady who was a woman older than 50, presented with what we call an atypical rash (even when it is more common, the atypical than the typical, we call it an atypical rash) and rather than improving in the first five days, the conduction system kept deteriorating. And I was telling her, according to my experience, when you get better, if you get resolved, I will not implant a pacemaker. We’ll do a stress test on the treadmill before you go home to show that there is full stability of the electrical system. But, by day four, the deterioration of the conduction system was even worse. So, I went to her room, and I explained to her that this was not working. So, now the consideration for implanting a pacemaker was on the table. I explained that I was going to give her one or two more days, but she may need a pacemaker. The next morning was the first ECG with what we call 1-1 conduction. That means that the upper chambers of the heart contract before the lower chambers of the heart and in a 1-1 fashion, and that is evolving towards normal electricity. So, we waited. We waited a couple more days. She re-assumed completely normal conduction by day 10 to 12. We put her on a treadmill, and she nailed it.
Of course, she was in excellent physical shape and so she presented with complete stability of her conduction system. So, she was discharged to complete a total of three weeks of antibiotics. After 10-12 days in the hospital with IV antibiotics, we switched to antibiotics by mouth. She was seen at 4-6 weeks doing her completely normal life. She’s coming to see us this coming week for her one-year follow-up—the first of eight patients with what we call long-term follow-up of properly treated Lyme carditis patients. This is a piece that doesn’t exist in the literature because basically what we all say is we treat them, we do well, they do well, we do not need a pacemaker. But nobody tells you what happens two, three years later. So, this lady is at about the 1.5-year mark. She will be included in this series that we hope to be submitted soon after we check on her physical examination, ECG, etc.
So far, the prior six patients have a minimum follow up of one year—maximum of 3.5—living an absolutely normal life without needing a pacemaker. And the important thing here is that not two decades ago, five years ago, any of these young individuals would have received a pacemaker for the rest of their lives. I make my living implanting pacemakers, right? But I don’t want any person in the world to have a pacemaker that they don’t need. The tip for my colleagues is this: patients who usually may be actively fit who present with unexpected AV blocks—which is this shutdown of the electricity in the heart—I would say to my colleagues: please consider Lyme disease. Before implanting a pacemaker, consider Lyme carditis. So, immediate serology. Initiate antibiotic treatments. And if there’s no other easy, detectable, transient cause to create an electrical problem, please consider this (Lyme carditis), because if you treat the symptoms with antibiotics, these patients—after a few weeks of antibiotics—may not require a pacemaker for the rest of their lives.
Remember. Pacemakers are batteries—batteries that we need to replace. And we do this all the time. But every time I open the skin to replace a battery, there’s a 2-3% risk of a serious infection that sometimes requires that we remove the whole system. With that in mind, here’s an example: A student who is one of these six patients is 19 years of age. If I implant him with a pacemaker, over the course of his life, this patient may have to have six or seven battery replacements at the cost of 2-3% risk of a serious infection every time I do that. So, I would much prefer to exchange that type of life with 10 days of admission and three weeks total of antibiotics.
So, when I have the (hospital) administrators asking me, “Adrian, why don’t you implant a pacemaker so I can discharge this patient?” I sit down and I show them the numbers. This is what you are going to do from a purely economic point of view. I’m not even saying that you may psychologically destroy the life of a teenager by implanting a pacemaker. Even when you convince them that they can have a normal life, they have a pacemaker. So, we have exchanged 10 days of admission—and I do recognize that there are costs associated with implanting a pacemaker, plus replacing the batteries six to seven times, plus all the things that imply living with a pacemaker.
Lia Gaertner: Obviously, in terms of economics, there’s a bottom line there that is clearly in favor of ruling out Lyme disease, which is more common than most doctors recognize. We also have a really tragic case of one of our favorite Duke University cancer and Lyme researchers who recently passed away, Dr. Neil Spector from undiagnosed Lyme carditis, where he actually went so far as having a heart transplant. And it was only after his heart was removed that they figured out that there were Lyme bacteria in his heart. What do you think it will take to get Lyme on the differential diagnostic radar for family medicine doctors, for cardiologists, and for anyone who might encounter somebody who’s having palpitations or arrhythmias or tachycardia, or feeling some of the symptoms that might come along with having some kind of Lyme carditis?
Adrian Baranchuk: What are the options for early disseminated Lyme carditis to progress? One, it gets properly diagnosed, treated, and we have demonstrated and published on this several times. I insist in the Journal of the American College of Cardiology and the Canadian Medical Association Journal, that if you recognize and treat (for Lyme carditis), the prognosis is excellent. And these people do very well. And these people do not require pacemakers. So, one of the options is that you diagnose, and you treat in this group what we still don’t know. And our next communication is going to be the first one in literature addressing this point: what happened in the long-term for the properly treated patients? We don’t know because I can give you a huge list of conditions that get properly treated. And then you have post-treatment Lyme syndrome. Dr. John Aucott from Johns Hopkins is the worldwide leader in understanding this concept of the long-term consequences of Lyme disease.
My colleague, Dr. Steven Phillips, along with Dana Parish, has just recently published a book called Chronic, which I’m very interested in reading because I want to understand all the perspectives, not only what Dr. Aucott brings me in the highest scientific level on post-treatment Lyme disease, but also the global perspective, the perspective from a patient, the perspective from a family on what it means to deal with clinical psychological deterioration and finding lots of barriers to find proper access. So, again, let’s review the three options:
- First group: You get cured. My lab is working on advancing knowledge of what happens in the long term for people that got properly treated.
- Second group: You did not get proper diagnosis and treatment. The disease evolves very rapidly and you die.
- Third group: And this is where the case of my colleague that unfortunately passed after receiving cardiac transplantation. Neil Spector died, which is rather than falling into the 90% of Lyme carditis that will evolve with electrical problems, you have a global problem if in your heart you have myocarditis, or even worse pancarditis, when the three layers of the cardiac wall are affected by Lyme. And that can produce a very sudden and rapid clinical deterioration leading to death, either during the acute episode, or as a consequence of complications of treatment received, including—in cases like Dr. Spector—cardiac transplantation. These are the three ways the condition evolves.
Now, all the studies conducted by Dr. Aucott in the long-term chronic phases of Lyme disease, have not focused on the heart and cardiovascular aspects of this condition. They know a lot about the autonomic nervous system that regulates our heart rate and blood pressure. They know a lot about joints, about muscles, about mental issues, but how the heart will be targeted in the long-term chronic manifestations of Lyme disease has never been properly investigated—to the point that we do not have a specific model for that. The first animal studies have been released in the last year or two to help us understand what are the things that can predict whether long-term cardiac consequences will occur after contracting Lyme disease.
You either have an early disseminated manifestation of cardiac electricity shut down. Or you have myo/pancarditis. I had to assist a lady whose 17-year-old daughter died on the day of her birthday. So this woman is going to spend the rest of her life every birthday remembering the death of her daughter because she couldn’t make it to cardiac transplantation. So, it was all on the phone trying to help the doctors. But once they realized it was too late, they couldn’t find the heart for her. There are gaps in knowledge, right? So, there could be long-term consequences of treating Lyme carditis that are not as serious as the early manifestation, but still produce palpitations, arrhythmia. There’s a beautiful paper from Poland in the American Journal of Cardiology 2020, showing atrial fibrillation, which is the most common arrhythmia linked to Lyme disease. So, I think they cite Lyme disease as a risk factor of atrial fibrillation or something like that.
Lia Gaertner: As you’ve mentioned, Lyme carditis is under-recognized, especially in many emergency departments, and patients need to visit the emergency department two to three times on average until the diagnosis is suspected. And, as we have seen, failure to recognize this may result in fatalities and illness. I know that you have developed a risk stratification tool called the Suspicious Index in Lyme Carditis, and it evaluates the likelihood that a patient’s high degree AV block is caused by Lyme carditis. And I was hoping that you could talk a little bit about that.
Adrian Baranchuk: We’re very happy because we see more and more publications now using the SILC score to stratify their patients and helping them to diagnose and manage these cases properly. So, the first thing to be said is—as a global message—a young individual younger than 50 years-old presenting with an unexpected complete heart block or high degree AV block, should raise the alarm to suspect Lyme carditis, and it should be part of the differential diagnosis. If other more common transient causes of AV block are present, such as having a heart attack? A heart attack can be complicated by a complete AV block or high degree AV block. But the ECG helps a lot in showing that you’re dealing with ischemia, which is a lack of oxygen in the cardiac muscle. So, then you can easily link that heart block to that heart attack and not put Lyme disease into context. However, if there’s no evident other cause for heart block, Lyme carditis should be part of your differential diagnosis.
To help healthcare providers, we designed the SILC score or Suspicious Index in Lyme Carditis, and it is an acronym that for people like me that love going to the movies is easy to remember, and it’s called COSTAR. So, in our COSTAR acronym, the C is for constitutional symptoms. That means fever, malaise, lack of appetite, lack of energy, all those things that separately may not mean a lot. But when you group them, we call them constitutional symptoms, and you receive points for having that. The O of the COSTAR is outdoor activities or endemic regions. This is people that usually expose themselves to areas where ticks are quite prevalent. The S is for sex, and as I said, the male gender is 8-9:1 with respect to females. The T is for tick bite. Some people do recollect having a tick bite. For example, in the case of this 56-year-old lady, she said to the doctors, “I think that I had a tick bite, but I couldn’t see the tick.” But that should raise the alarm: “You think you had a tick? You think you removed a tick, or you did remove a tick?” That is an alarm to put into the context of a high degree AV block. I could say that a tick bite and a high degree AV block or typical rash and high degree AV block equals Lyme in any part of the world. So that’s the T. The A is for age—people under 50 years old, and the R is for the rash, the so-called erythema migrans or “bullseye” rash, which is present in people with Lyme carditis, not more than 30-40% of the time.
But as I said, if you have the typical rash on a high degree block, that’s Lyme until you demonstrate otherwise. So, that is the COSTAR and the COSTAR assigns different points to the variables. When you have 3-7, which we call intermediate, or 7-12 that is what we call a high probability of Lyme carditis—when you should take blood samples for Lyme serology and treat the patient with IV antibiotics and have the patient on a monitor system. If this low cardiac rhythm that we call bradycardia is quite excessive and the patient is not tolerating, you may need to consider implanting a temporary pacemaker.
I’m going to tell you something that we are currently navigating. There are two patients that were referred to me that during the acute phase of their electrical shutdown; they were implanted with pacemakers. Subsequently, within a week, serology returned positive for Lyme disease. Both of them were properly treated with more than three weeks of antibiotics. Remember that a pacemaker can store the information of every single beat for longer periods of time. In the first case I had the opportunity to see approximately three months after the device insertion, the patient was using it since it was implanted until the second day of receiving the first dose of antibiotic IV. And since then, until three months later, I interrogated the device in our hospital, the patient has not used the pacemaker at all.
So, now I have a patient that was properly treated with the right doses of antibiotic in her particular case. This is my second woman. The dose was even larger than what the CDC recommends as the proper dose of antibiotics. So, we had a long discussion, and I did all the tests that I could do to her before implanting the pacemaker. And all the tests were normal. She was able to do a treadmill with a heart rate of 168 beats per minute with 1:1 conduction. So, we entertained a discussion of what it would take to remove the pacemaker. I’m happy to report to you that three weeks ago we explanted (removed) her pacemaker. She is doing absolutely fantastic. I’ve been in contact with a company in the US to try to analyze the tips of those devices to see if there is any remaining bacteria component in those cells that could be in the tip of the device.
And I am seeing in the next week the second patient with exactly the same story. So, this is to reinforce to my colleagues that if you learn the SILC, if you apply the SILC, please think Lyme carditis to avoid having to go through all this trouble of explanting—in the best possible case—explanting the pacemaker because the patient finally got treated and avoiding implanting the pacemaker in the first place if the patient responded well to antibiotics. So, of course that this is going to open another report because to the best of my knowledge, at least in a systematic manner, by studying the heart condition of the patient before deciding the extractions for properly treated Lyme carditis have not been done before. So, as soon as this is out, I will be sure to contact you so I can send you the new material.
Lia Gaertner: And Lyme disease antibody testing is far from a perfect science. So, when you get all those variables, and it’s a lot of uncertainty, and it sounds like there needs to be a lot more research.
Adrian Baranchuk: I’m so happy that we have universities like others of course, such as Johns Hopkins, working on giving us better tools. It is a much-needed field of medicine to advance a universal way of testing for Lyme that we don’t need to wait five to seven days. Lyme carditis is the best example of why we need this in 24 hours which gives us a full understanding of whether there’s, a)persistence of bacteria or more than one bacteria—because you know that there are several co-infections, b) persistence of bacteria in the body, and c) antibodies that have been developed. We need better tests, more accurate tests.
We know, and this is not new, in the early nineties, there was a New England Journal of Medicine paper called Non-Serology Lyme Disease. So, when you have Lyme disease, the serology returns as negative. Of course, we have learned a lot of stuff since then. We’ve learned about co-infections. But I could tell stories of patients presenting with classic Lyme carditis improving on antibiotics and the serologies returning negative, right? And this was in the time where I wasn’t sure about Babesia, about other infections that could be producing the same thing, responding to the same antibiotic, but being negative for the serology, right? And some of those stories rather than being comic are quite tragic because when doctors don’t see the positivity of the serology, they are reluctant to keep treating patients for the three weeks that we’ve proven to be effective for antibiotic treatment.
I am very glad that finally the CDC has a segment in its Lyme disease website about Lyme Carditis. One can argue how to format that segment of the website, but the truth is that it is there and that the information provided is completely accurate and useful. I would love them to replicate the only existent algorithm for management of Lyme carditis that is published in JACC, but they included the reference to that paper. If they contacted me, I could grant them permission for reproduction of that figure so people can see it and have a visual impact. But the fact that they are using it as their recommended lectures made me on a personal level very happy. But I commend the CDC for having included a segment on Lyme carditis that moves in the right direction. So, with this type of attitude from NGOs, from families, from scientists, and from organizations, if we can build bridges and work together is how we’re going to win this condition.
Lia Gaertner: Thank you so much Dr. Baranchuk for joining us today on the Ticktective video and podcast series. We really appreciate what you’re doing for people with Lyme carditis and various cardiac manifestations of tick-borne disease. And we are very grateful that you are an outspoken advocate. And thank you so much for joining us.
Adrian Baranchuk: Thank you so much, Lia, for having me here. It was a real pleasure talking to you, and I remain at your disposal for further conversations.
Lia Gaertner: Thank you for joining us for this episode of the Ticktective podcast and video series, a program of the Bay Area Lyme Foundation. You can find out more or donate@bayarealine.org.
This blog is part of our BAL Spotlights Series. It is based on a transcript from Ticktective, our podcast and video series. To listen or watch the original conversation, please click here. Bay Area Lyme Foundation provides reliable, fact-based information so that prevention and the importance of early treatment are common knowledge. For more information about Bay Area Lyme, including our research and prevention programs, go to www.bayarealyme.org.


I forgot to mention my Cardiac symptoms , which seem to be controlled with medication although , the medication I think is primarily to prevent Syncope which became a problem several years ago . Testing showed that I have a dilated Aorta and Aortic root
Hi, my name is Brian . I live in MPHS TN . I have been ill since 1987 . I was bitten by a Tick in the spring of that year .I started having symptoms shortly there after .Jump forward 35 years . I had to retire from my job in 1999 due to Hemianopsia and memory problems .I was treated in 1999 with I.V . Rocephin and my vision improved immediately although my joint and sensation problems did not . He gave me all the IV treatment the insurance would cover . I have had Knee replacement and two disc replaced in my neck ACDLF .The last Infectious Doctor I saw told me “You don’t have Lyme Disease , there’s no Lyme Disease in this area” That was several years ago . Thank you for your time . Brian