Ticktective Podcast Transcript
In this conversation between Ticktective™ host Dana Parish and pioneering physician Kenneth Liegner, MD, the discussion focuses on how Dr. Liegner, frustrated and perplexed by the lack of options for persistent/chronic Lyme, came to prescribe disulfiram—a drug intended to treat alcoholics—as an off-label therapeutic for his Lyme patients. He recounts what happened next, and reflects on the impact of his bold experiment, plus they touch on how a Covid infection may impact Lyme patients, causing a resurgence of latent symptoms. They also explore the history of tick-borne diseases and the lack of recognition among clinicians, the government, and insurance companies for these insidious infections that cause chronic suffering for many. Note: This transcribed podcast has been edited for clarity.
Dana Parish: Welcome to the Ticktective Podcast, a program of the Bay Area Lyme Foundation, where our mission is to make Lyme disease easy to diagnose, and simple to cure. I’m your guest host today, Dana Parish. I’m the co-author of the book Chronic, and I’m on the advisory board of Bay Area Lyme Foundation. This program offers insightful interviews with clinicians, scientists, patients, and other interesting people. We’re a non-profit foundation based in Silicon Valley, and thanks to a generous grant that covers a hundred percent of our overhead, all of your donations go directly to our research and our prevention programs. For more information about Lyme disease, please visit us at bayarealyme.org.
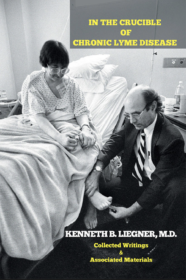 Dana Parish: I’m so thrilled to be guest hosting Ticktective for you today on behalf of Bay Area Lyme Foundation. I’m here with a dear friend and a brilliant Lyme physician, internist, author, Dr. Kenneth Liegner. Dr. Kenneth Liegner is a board-certified internist with additional training in pathology and critical care medicine, practicing in Pawling, New York. He’s the author of an extraordinary documentarian history of Lyme called In the Crucible of Chronic Lyme Disease, Collected Writings and Associated Materials. We’ll talk about that more later. Dr. Liegner is also the first to apply disulfiram in the treatment of Lyme, and he published his experience in the peer-reviewed journal Antibiotics. Thank you so much for being here with me today, Dr. Liegner.
Dana Parish: I’m so thrilled to be guest hosting Ticktective for you today on behalf of Bay Area Lyme Foundation. I’m here with a dear friend and a brilliant Lyme physician, internist, author, Dr. Kenneth Liegner. Dr. Kenneth Liegner is a board-certified internist with additional training in pathology and critical care medicine, practicing in Pawling, New York. He’s the author of an extraordinary documentarian history of Lyme called In the Crucible of Chronic Lyme Disease, Collected Writings and Associated Materials. We’ll talk about that more later. Dr. Liegner is also the first to apply disulfiram in the treatment of Lyme, and he published his experience in the peer-reviewed journal Antibiotics. Thank you so much for being here with me today, Dr. Liegner.


 In this conversation between Ticktective™ host Dana Parish and Harvard-trained
In this conversation between Ticktective™ host Dana Parish and Harvard-trained 










 Guest Post from
Guest Post from