FOR IMMEDIATE RELEASE
Science Translational Medicine Study Funded by the Bay Area Lyme Foundation Identifies FDA-approved Piperacillin as More Effective, Targeted Treatment for Lyme Disease
An additional Science Translational Medicine study also funded by Bay Area Lyme Foundation uncovers how lingering bacterial cell wall molecules may contribute to chronic Lyme symptoms
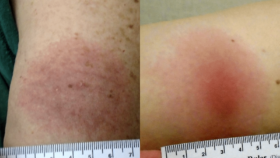
PORTOLA VALLEY, Calif. April 23, 2025 – Bay Area Lyme Foundation, a leading sponsor of Lyme disease research in the US, announces two pre-clinical studies published in the peer-reviewed journal Science Translational Medicine. The studies demonstrate promising implications for improved Lyme disease treatment and understanding of chronic Lyme through peptidoglycan, a molecule found in the cell wall of the bacterium, Borrelia burgdorferi (Bb), which causes Lyme disease. The first study finds piperacillin, an FDA-approved treatment for pneumonia that inhibits peptidoglycan production, may be a more effective treatment for Lyme disease than the current “gold standard” treatment, doxycycline, which is not effective for up to 20% of patients. The second study uncovers how lingering peptidoglycan builds up in the joint fluid and liver, contributing to chronic Lyme symptoms, which affect over 20% of patients treated for Lyme disease.
“Piperacillin may be a game-changer for improving Lyme disease treatment, which is currently a challenge for researchers and physicians. Furthermore, our new mechanistic understanding of how piperacillin affects peptidoglycan synthesis is unexpectedly informing our development of a biomarker-based approach to diagnose acute Lyme disease,” said Brandon Jutras, PhD, associate professor of Microbiology-Immunology at Northwestern University Feinberg School of Medicine, and a Bay Area Lyme Foundation 2021 Emerging Leader Award winner. “Our second study explores the role of peptidoglycan in chronic Lyme symptoms; peptidoglycan influences an inflammatory and chronic illness response for weeks or even months after infection, adding to the growing evidence that remnants of bacteria and viruses can stick around and keep affecting the body, similar to the occurrence of Long COVID in some patients.”



 Ticktective host, Dana Parish, talks with her longtime collaborator and co-author of
Ticktective host, Dana Parish, talks with her longtime collaborator and co-author of 

 “I want to leave you with hope. I think we’re going to be unstoppable because I think that these are solvable problems. These are answerable questions. I think that there are already a lot of existing tools in immunology that just need to be brought into the fight, and we can change this.”
“I want to leave you with hope. I think we’re going to be unstoppable because I think that these are solvable problems. These are answerable questions. I think that there are already a lot of existing tools in immunology that just need to be brought into the fight, and we can change this.”  Any respectable pathogen that can establish a persistent infection needs to figure out your immune system to the point that it can evade it. The fact that it has persisted means that it was able to evade your immune clearance. And so, I got to that from a very interesting direction working on immune regulation, trying to understand these brakes on the immune response and how they impact the response to infection. The immune system has the power to kill you and obviously, nobody has any incentive for that to happen. So, there are a lot of mechanisms in place to put brakes on the immune system and reign it in. One of the huge developments in cancer over the last two decades has been reevaluating the question: can we take those brakes off? So in my postdoc, I was studying a particular checkpoint where this was turning into an exciting immuno-oncology target, and I said, ‘I want to look at how this checkpoint is used in infection.’ I realized that this checkpoint was being used to help you survive an acute infection, but created a vulnerability for pathogens to evade immune clearance and establish chronic infection much like it allows cancer cells to evade immune clearance. In an amazing collaboration with Irv Weissman, Balyn Zaro, and Jenifer Coburn we realized that the bacteria that cause Lyme disease manipulate this brake and that’s how I became fascinated with Lyme. But I also became concerned about turning off this brake in cancer patients because I was concerned about what would happen if you used this on cancer patients during an active infection. Indeed, the
Any respectable pathogen that can establish a persistent infection needs to figure out your immune system to the point that it can evade it. The fact that it has persisted means that it was able to evade your immune clearance. And so, I got to that from a very interesting direction working on immune regulation, trying to understand these brakes on the immune response and how they impact the response to infection. The immune system has the power to kill you and obviously, nobody has any incentive for that to happen. So, there are a lot of mechanisms in place to put brakes on the immune system and reign it in. One of the huge developments in cancer over the last two decades has been reevaluating the question: can we take those brakes off? So in my postdoc, I was studying a particular checkpoint where this was turning into an exciting immuno-oncology target, and I said, ‘I want to look at how this checkpoint is used in infection.’ I realized that this checkpoint was being used to help you survive an acute infection, but created a vulnerability for pathogens to evade immune clearance and establish chronic infection much like it allows cancer cells to evade immune clearance. In an amazing collaboration with Irv Weissman, Balyn Zaro, and Jenifer Coburn we realized that the bacteria that cause Lyme disease manipulate this brake and that’s how I became fascinated with Lyme. But I also became concerned about turning off this brake in cancer patients because I was concerned about what would happen if you used this on cancer patients during an active infection. Indeed, the 

 Charlotte Mao:
Charlotte Mao:
 Anna Schotthoefer, PhD, a project scientist at Marshfield Clinic Research Institute in Wisconsin, discusses the collection and analysis of a specific subset of blood and urine samples for Lyme Disease Biobank—a Bay Area Lyme Foundation program—from patients diagnosed with tick-borne diseases in the state. Marshfield Clinic serves a large population in Wisconsin and Michigan’s Upper Peninsula, which are highly endemic for Lyme disease. Her Bay Area Lyme-funded
Anna Schotthoefer, PhD, a project scientist at Marshfield Clinic Research Institute in Wisconsin, discusses the collection and analysis of a specific subset of blood and urine samples for Lyme Disease Biobank—a Bay Area Lyme Foundation program—from patients diagnosed with tick-borne diseases in the state. Marshfield Clinic serves a large population in Wisconsin and Michigan’s Upper Peninsula, which are highly endemic for Lyme disease. Her Bay Area Lyme-funded