Ticktective Podcast Transcript
In this conversation with Dana Parish, Todd Maderis, ND, talks about his extensive experience treating tick-borne infections, chronic viral infections, mold illness, and other conditions associated with complex chronic illness. He underscores the significance of identifying the root causes of symptoms and how tailoring individualized treatment approaches is key to healing. Dr. Maderis also delves into the role of trauma in chronic illnesses and emphasizes the importance of gut healing and inflammation reduction through dietary choices. Dr. Maderis acknowledges the challenges involved in addressing chronic diseases and stresses the importance of a personalized, patient-centric approach.
“I think a lot of times in conventional medicine, we don’t think beyond the room that we’re sitting in with a patient, we have to ask about the environment. We have to look at more than just the symptoms the person’s presenting with in the office.”
– Todd Maderis
 Dana Parish: I am so excited today because I’m here with Dr. Todd Maderis. Thank you so much for being here today. I’m thrilled to talk to you. Let me tell you a little about Dr. Maderis. He’s the founder and medical director of Marin Natural Medicine Clinic in the San Francisco Bay Area. He specializes in treating tick-borne infections, chronic viral infections, mold illness, and other conditions associated with complex chronic illness such as Mast Cell Activation Disorder, and ME/CFS. His approach to treating chronic illness is to identify all underlying causes of symptoms to provide a clear direction for treatment. With over a decade of experience treating Lyme disease and complex chronic illness, he knows that every patient is unique and requires individualized treatment therapy. Welcome! It’s great to see you!
Dana Parish: I am so excited today because I’m here with Dr. Todd Maderis. Thank you so much for being here today. I’m thrilled to talk to you. Let me tell you a little about Dr. Maderis. He’s the founder and medical director of Marin Natural Medicine Clinic in the San Francisco Bay Area. He specializes in treating tick-borne infections, chronic viral infections, mold illness, and other conditions associated with complex chronic illness such as Mast Cell Activation Disorder, and ME/CFS. His approach to treating chronic illness is to identify all underlying causes of symptoms to provide a clear direction for treatment. With over a decade of experience treating Lyme disease and complex chronic illness, he knows that every patient is unique and requires individualized treatment therapy. Welcome! It’s great to see you!
Todd Maderis: Thank you for having me. It’s great to be here.
Dana Parish: How’d you get into this mess?
Todd Maderis: Gosh, that’s always a great question. You start going down a rabbit hole and sometimes you wonder, but I wouldn’t change a thing. My first five years of practice, I was treating people with common complaints: digestive issues, fatigue issues, thyroid issues, etc. I’m a naturopathic doctor, so we tend to see people that come with common complaints that maybe they’re not getting resolved in conventional medicine. Then one visit, I had a patient that brought in a Lyme disease test result. It was an iGenex test, but back then the results were pretty hard to interpret.
Dana Parish: What is iGenex for people who are new to hearing about them?
 Todd Maderis: iGenex is a Lyme testing specialty laboratory here in the San Francisco Bay Area. They have been doing testing for tick-borne infections for over 30 years. In my opinion, they offer the gold standard for testing for tick-borne infections. The results at the time were hard to interpret. I couldn’t make heads or tails of them. Around the same time, a colleague had told me about a Lyme conference, and the next thing you know, I was on a flight to a conference. At the time it was a small conference. There were very few of us in the audience and a lot of great speakers and—as you know—once you learn something, it’s hard to unlearn it or it’s a little negligent to pretend that it’s not there. That really changed the course of my practice. Then of course, you really learn from your patients. People come in with different complaints or maybe what you’re addressing is not resolving their symptoms, so you keep searching. And I think in medicine, you have to be curious. It’s important to stay humble as well because you get surprised, and you learn things. And yes, my practice has evolved over the years, and I wouldn’t change a thing. What I’m doing now, I really enjoy it.
Todd Maderis: iGenex is a Lyme testing specialty laboratory here in the San Francisco Bay Area. They have been doing testing for tick-borne infections for over 30 years. In my opinion, they offer the gold standard for testing for tick-borne infections. The results at the time were hard to interpret. I couldn’t make heads or tails of them. Around the same time, a colleague had told me about a Lyme conference, and the next thing you know, I was on a flight to a conference. At the time it was a small conference. There were very few of us in the audience and a lot of great speakers and—as you know—once you learn something, it’s hard to unlearn it or it’s a little negligent to pretend that it’s not there. That really changed the course of my practice. Then of course, you really learn from your patients. People come in with different complaints or maybe what you’re addressing is not resolving their symptoms, so you keep searching. And I think in medicine, you have to be curious. It’s important to stay humble as well because you get surprised, and you learn things. And yes, my practice has evolved over the years, and I wouldn’t change a thing. What I’m doing now, I really enjoy it.
Dana Parish: Well, it’s been nice to have a relationship with you over these last couple of years and know that I could talk to you about toxic mold, about chronic Lyme, about Long Covid, and about all the other immune assaults that we face just living in the world today and being able to send you patients with all these different complex issues that you’ve been able to unravel. One of the things I’m really excited to talk to you about is toxic mold. I think it is hugely underappreciated all over the world, and it’s a big problem all over the world, and I think doctors don’t really know how to look for it. I’m curious what your experience is and how you came to recognize it as such an important factor in the chronic illness world.
“I think in medicine, you have to be curious. It’s important to stay humble because you get surprised, and you learn things.”
– Todd Maderis
Todd Maderis: Yes. I sometimes joke, if you told me 10 years ago, I would be treating mold illness I would have been amazed. At the time, I didn’t know what it was, but about 10 years ago, I was at a large international Lyme conference, and I remember looking at the lineup of speakers for the weekend, and typically all the talks are related to Lyme or co-infections. And there was one speaker in the lineup that was talking about mold illness—an infectious disease doctor named Joe Brewer from Oklahoma. And at first, I thought he’s in the wrong place. This is the wrong conference. After hearing his talk, I learned that toxic mold or mold illness can present very much like Lyme and mold.
Dana Parish: Tell us some of the symptoms because I think, again, people have no idea what we’re talking about.
Todd Maderis: I think what’s important is to make a distinction. In conventional medicine we talk about mold allergy, right? Occasionally I’ll see someone that’ll say, “Oh, my primary care physician tested me for mold, but it was normal.” It was a LabCorp test and they tested for it, but those are mold allergies. So, that’s an antibody test to detect a mold allergy. We have mold allergies. But we also have mold illness, and then people can have more serious conditions like pulmonary aspergillosis. What we’re referring to is an elevation of mycotoxins, which are a secondary metabolite of mold. So, when people get exposed to water damaged buildings—that’s the term that’s used—we inhale mold spores. And those mold spores can colonize humans, typically in the sinus cavity or the GI tract, and they’ll continue to make mycotoxins. These molds will produce mycotoxins well after someone has left that moldy environment.
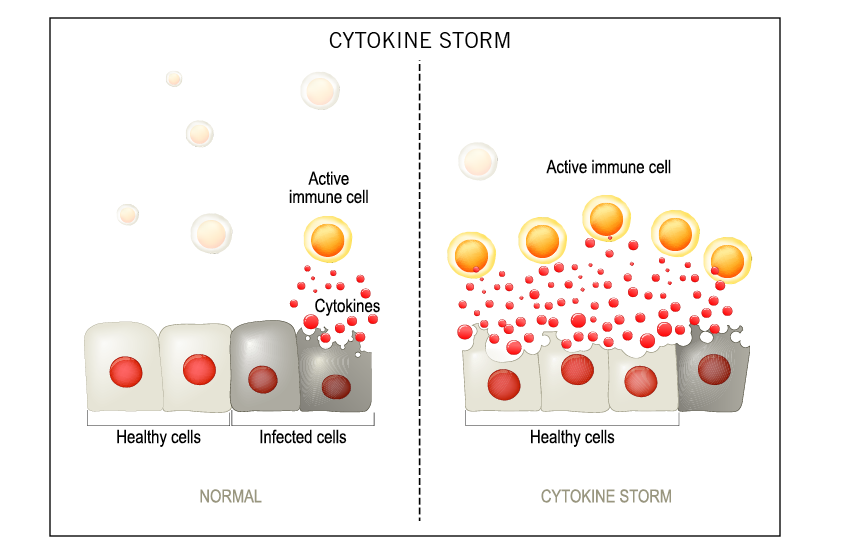
It’s similar to Lyme, right? You could have a tick bite five, 10, or 15 years before you develop symptoms. Then something happens—almost that perfect storm—and sometimes mold is part of that perfect storm because mold is very immunosuppressive. So, when I talk about mold illness, the symptoms can range from fatigue and brain fog, headaches, anxiety, depression, to respiratory symptoms, to arthralgias, aches and pains. There’s a myriad of symptoms that can come because essentially the toxin is triggering an immune cytokine response. So, there isn’t just an allergy type of symptom or a respiratory only symptom. It’s a systemic multisystem, multi-symptomatic illness similar to mold.
“You could have a tick bite five, 10, or 15 years before you develop symptoms. Then something happens—almost that perfect storm—and sometimes mold is part of that perfect storm because mold is very immunosuppressive.”
– Todd Maderis
Dana Parish: I think people don’t appreciate that if they’re living in a moldy environment and there are mycotoxins, they’re airborne, they’re microscopic, and you’re inhaling them and you’re getting neurologic symptoms. It’s sort of like the Lyme thing, right? People think that it’s just arthritis, but no, it’s totally not. It also goes into your brain, and you have neurologic symptoms. And it’s deeply disturbing to me to find out what I have learned in the last couple of years about toxic mold. I didn’t know that it could be used as a bioweapon. As Dr. Charlotte Mao has said to me, these are true poisons and I think they’re really under-appreciated. So, if you suspect a patient has been exposed and one of the problems that’s affecting them is toxic mold, what do you do?
Todd Maderis: Well, it always starts with a history. Rarely do people walk in the door and know that they have mold exposure. Occasionally someone will suspect it, and of course my practice is specialized, and so people may seek me out for that diagnosis, but people typically aren’t aware of it. Mold does not like light. It doesn’t tend to grow out where we can see it. What is factored into a rise in mold illness, maybe in the last five decades, is that construction has probably played a role. We now have cavities in every wall, which are a perfect source or location for mold growth. So inside of walls where it’s dark and damp, mold likes to grow, it doesn’t typically grow out where we can see it. I once had a patient, a Lyme patient at the time who had moved to Brooklyn, and she hung a painting on the wall when she moved into her apartment.
And within three months she got really sick, and she had to move back home to San Francisco to live with her parents. When she left the apartment, she took the painting off the wall, and mold had grown in the shape of the painting. The mold was already there. The moisture inside of the wall was there and where she had blocked the light with a painting, mold had grown. And so, mold tends to lurk in places. It doesn’t have to be obvious like a roof leak where you see a water stain on the ceiling, toilets overflow, bathtubs overflow, dishwasher leaks, washing machines, crawl spaces, etc. I’m in Marin County, just north of San Francisco, and we have a lot of hills and beautiful redwoods. Some homes are built in canyons with redwood trees, so there’s a lot of dampness.
We also have homes that are built on bedrock in Tiburon, and water just flows down the hill when it rains and doesn’t really seep in. So, things like basements are red flags. Anything that’s subterranean or hillside, the HVACs get affected by mold growth. And then every time you turn on the HVAC, it can disseminate these mycotoxins. To your earlier point, they are microscopic. Mycotoxins are about the size of a virus. I mean, they’re extremely microscopic and they waft around the house. People will say, “Oh, we found mold in my daughter’s closet, and so we’re fixing that.” And I once heard an analogy about mold spreading throughout the house, sort of like if someone was cooking in the kitchen and they were cooking bacon, for example, and you can smell it down the hallway. Mycotoxins are doing that. They’re not isolated in that one room in the building. We could have a six-hour podcast about the whole building issue because it really is one of the greatest obstacles to helping people get better.

I’m in the San Francisco Bay area and we have 8 million people here, and there’s really one or two inspectors that I trust to inspect the home properly. I mean, it’s a whole art and science. Same thing with remediation. I would say a majority of the time when people remediate, it’s done improperly. We often say mold needs to be removed, not killed. Occasionally I’ll talk to someone, and they’ll say, “Oh, they just came in and they painted over with this paint that kills off mold, or they sprayed something, some eco-friendly antiseptic cleanser,” and you don’t ever want to do that. In fact, when you disrupt mold, it gets angry, and it releases more mycotoxins. Mold is like skin cancer; it should always be removed with clean margins. And I often say there’s a thousand ways to do it wrong and very few ways to do it right. Diagnosing in humans is one thing. They come in; I get the thorough history. It may come up or not on the tests.
Dana Parish: Do you feel you can rely on good tests?
Todd Maderis: For sure. I’ve used a variety of them over the years. I’ve cycled through a lot of tests in the last decade and used a whole variety of testing. Right now, I’ve locked in on using urine mycotoxin testing and a lab out of Texas is my preferred lab.
Dana Parish: What’s it called? The lab?
Todd Maderis: Real Time Labs in Texas. It’s actually the first lab I ever used 10 years ago. And then the details are everything, right with testing. And the same thing with Lyme testing and treatments is the same way. We start out by provoking mycotoxins with glutathione because mycotoxins need to be mobilized to capture in the urine so that we get an accurate sample. We typically give patients an IV of glutathione the day before they collect, but a lot of people don’t have access to IVs. They can use oral glutathione for five days beforehand.
Dana Parish: That’s great to know. That’s a helpful tip actually. It’s very complicated and it’s extremely expensive. The problem with all of these things is that because they’re purposely outside insurance coverage, insurance companies don’t want to pay for mold remediation because they found out in the late 1990s, early 2000s how incredibly expensive it can be, and the liability can be tens of millions of dollars. As you and I have discussed, there are a couple of these famous cases where the whole family was poisoned. These multimillion-dollar homes are just absolutely infested. I spoke with somebody yesterday who just fled their gorgeous LA mansion in the middle of the night and had nowhere to go and they had to leave their things behind because they feel ill when they’re around them. The first time I heard these kinds of stories, I was very skeptical.
Really? You can’t take your sofa. What if you just get it steam cleaned? Actually, it turns out they were right. And when you think about it, at some point, I was talking to a doctor about it and we were talking about the comparison to Permethrin, right? You can pre-impregnate your clothes and then you can launder them many times and you still have the permethrin. And it’s hard to imagine that that’s possible and yet it is. I now think of mycotoxins as being that hard to get rid of sometimes. And people are becoming extremely sensitive.
Todd Maderis: Yes, especially when the patients are extremely sensitive to everything around them. They almost have to leave all their belongings behind. Anything porous that really absorbs mold—mattresses, for example, I often say are sponges for mold. If people identify mold in their current location, they move into another location that’s clean. If they take their stuff with them, they’ve contaminated their new environment. So, it does become very challenging. It’s extremely costly. It creates a rift with family members because there may be people in the household that aren’t sick, and so husbands may not understand why their wife is so sick and sensitive. I often say that when I diagnose someone with mold illness, it’s a real benefit to everyone in the household, and I’m just glad that it extends the benefit to everyone else that’s living there because they may or may not know about it.
One of my patients currently has an autoimmune condition, a scleroderma-type condition, and her husband’s fine. He got very sick with Covid during the pandemic, and he had a cardiovascular event. He’s in his early fifties and he’s a former collegiate athlete, so he was very fit. I don’t know if it was a stroke or a heart attack, but he became very, very sick with his Covid illness. Well, when I met her, she already knew there was a past history of mold in the house and it was remediated, so she didn’t even bring it up. And then on testing, she had really high levels. She’s being treated at UCSF by a rheumatologist for this condition. The medication he has her on is called CellCept. And if you know anything about CellCept, it’s an immunosuppressive drug that’s used in organ transplants and to prevent rejection. And CellCept is derived from one of the mycotoxins, so it comes from mycophenolic acid, and I think that just demonstrates how immunosuppressive these mycotoxins are, right? If drug companies put it in a pill and sell it to suppress the immune response, clearly these mycotoxins are just extremely immunosuppressive.
Dana Parish: That’s fascinating. I didn’t know that. Is she able to tolerate the drug or is it impossible now that there’s this mycotoxin?
Todd Maderis: It does suppress inflammation, but ironically, she hasn’t felt any better on the medication, but her disease was progressing and so she had taken it for 30 days with no response, so she stopped it on her own, but her disease progressed. So, she’s sort of hedging her treatment right now. She’s on it while we’re also addressing the underlying issue. And as I shared with her, you could stay on this medication, but the mold is still going to be in your system.
She still has that in her body, and she had her house retested. Often what doesn’t happen is after home is remediated, and in her case, it was remediated years ago before I knew her, but people don’t retest after remediation. It’s like treating a condition. If someone has Lyme, you diagnose it and then you treat them for a period of time, but you always want to do follow-up testing. The house just got retested and sure enough, the remediation wasn’t done properly. It could be a rabbit hole; it could be very costly for people. Unfortunately, I see people that are renters and of course landlords don’t want to take on remediation or do much about it. At times, people’s hands are tied, and they get stuck in situations that are difficult to get out of. And that I think is one of the hardest parts about mold illness. It involves an outside building that is different from just treating the person that’s sitting with you in your office. You have to take into consideration their environment. And I think a lot of times in conventional medicine, we don’t think beyond the room that we’re sitting in with a patient, we have to ask about the environment. We have to look at more than just the symptoms the person’s presenting with in the office.
Dana Parish: What are a couple things people should know? Say you take a test, and you find out that you have been exposed to a high level of mycotoxins. Where do you start? If you can do a couple of things on your own, some doctors say the most important thing is to get out of the environment. What is true in your opinion?
Todd Maderis: With a multimillion-dollar mansion and people having to flee, there can be different severities of water damage. You can almost think of it as an infection. There’s a certain load or burden that comes into play. On low levels, pathogens may not cause an infection. An infection is really when it establishes itself and causes issues. With mold and water damage I think that if people are in a severely damaged environment, they do need to get out. If it is low level and can be remediated, then I think that’s the best-case scenario. People love where they live and it’s almost heartbreaking to hear that you might have to move or how do you tell your loved ones that this is what you’re doing?
Reducing exposure is always step number one. When they’re in their environment, people can also use air purifiers. They can open windows more frequently and cross ventilation or air exchange is important. We can do that in California for a good 10 months out of the year, maybe less, but you can’t do that everywhere. Ultimately, reducing your exposure is the goal. People then often use things like binders. Binders are taken orally, things like charcoal and clay, and humic and fulvic acids, and these mycotoxins are excreted in the bile. With a binder in the intestine, it binds up the mycotoxins and pulls it out of the body. We use a lot of glutathione to treat mold illness as well because that facilitates clearance. I just presented a few months ago at a conference on the pathophysiology of mold illness, and as I was preparing that presentation, I dove into all the research and looked at the mechanism of injury of mold or mycotoxins, and I had an “Ah-ha” moment halfway through all this literature, and I thought that when you look at some of the collateral damage that occurs, we have things like oxidative damage is probably the main mechanism of injury, and that can affect things like mitochondrial function and cell membrane health and organ systems. We also know mycotoxins trigger a lot of immune system dysfunction. There are really great studies out there on cytokines that are elevated. I think we once posted in my social media a side-by-side of cytokines triggered by Lyme and cytokines triggered by mold, and they’re almost identical. So, there’s a lot of immune system dysregulation, which is where these symptoms come from. As I’m reviewing this literature, I think, “Okay, if I’m pulling the mold out, but this oxidative damage has occurred, we know blood-brain barrier can break down, mitochondrial dysfunction occurs. There’s increased risk of neurodegenerative conditions like MS and Parkinson’s.” Then it’s also my responsibility to help my patients heal from that. So, a light bulb went off and I realized it wasn’t just detoxification. There’s also a healing piece that needs to come into play.
Dana Parish: Are there things you can recommend for people who are just beginning this journey to talk to their doctors about. We’re hearing a lot about mitochondrial dysfunction in the face of Covid. It’s something that is sort of in the mainstream because people are getting very severe ME/CFS-like symptoms from Long Covid. You and I again have talked about this before privately, just the number of athletes, the number of so-called healthy young people that are being struck down by this. And there’s a lot of talk about this being related to persistent infection. We know there are 300-400 studies now on Long Covid. You and I talked about the review recently in Nature that Amy Proal and her team and Rudy Tanzi at Harvard, they all came together and put this review out recently. So, there’s persistence, there’s potentially mitochondrial dysfunction. Where do you even begin and what can you do for these things? What can you do for mitochondria?
 Todd Maderis: It’s a process for sure. People will take oral supplements for mitochondria, things like NAD (nicotinamide adenine dinucleotide). I think it’s also because mitochondria has a structure and not just a function. More recently we’ve been sending blood to a lab in Germany that assesses mitochondrial function, cell membrane health, and mitochondrial membrane health. That’s been helpful to help guide patients in their treatment. We use a lot of IV therapy in my practice just because I find it works most effectively. I see really sick patients, and so oral supplementation can get you so far, but we typically do complex IV protocols that really include a lot of phospholipids, like phosphatidylcholine that help repair cell membrane damage.
Todd Maderis: It’s a process for sure. People will take oral supplements for mitochondria, things like NAD (nicotinamide adenine dinucleotide). I think it’s also because mitochondria has a structure and not just a function. More recently we’ve been sending blood to a lab in Germany that assesses mitochondrial function, cell membrane health, and mitochondrial membrane health. That’s been helpful to help guide patients in their treatment. We use a lot of IV therapy in my practice just because I find it works most effectively. I see really sick patients, and so oral supplementation can get you so far, but we typically do complex IV protocols that really include a lot of phospholipids, like phosphatidylcholine that help repair cell membrane damage.
And another phospholipid called phosphoethanolamine are the two main phospholipids in the mitochondrial membrane. That’s part of the repair process that needs to occur. And phosphatidylcholine also helps detoxify and clear out these mycotoxins. You’re essentially displacing the mycotoxins that have embedded in cell membranes and helping remove them. So that’s become a really big part of my practice, not just for mold patients, but for any chronically ill patient that this damage occurs. When I look at these results, I go, “Wow.” Then with a younger person, someone in their twenties or thirties, we’re seeing mitochondrial and cell membrane damage that you would typically see with age. And you’ve heard when people are older and they get diagnosed with a condition, and they’ll say, “Well, the neighbor down the road, he got Parkinson’s, but he is 76, and so it’s bound to happen.” It’s accepted to happen later in life or cancer or whatever—fill in the blank. It dawned on me that chronic illness is almost advanced aging. These pathogens or toxins that people are exposed to, cause damage that speeds up the aging process. And that’s why a 30-year-old person can be completely bed-bound with fatigue from the collateral damage from an infection or toxin.
In my practice, I feel it comes down to those two things. If you keep asking why and you and you see all these other associated conditions—whether it’s mast cell activation syndrome or these peripheral conditions—if you keep asking why, eventually you get down to an infection or a toxin or both—at least in my practice.
“Chronic illness is almost advanced aging. These pathogens or toxins that people are exposed to, cause damage that speeds up the aging process. That’s why a 30-year-old person can be completely bed-bound with fatigue from the collateral damage from an infection or toxin.”
– Todd Maderis
Dana Parish: The diagnoses in and unto themselves and everything has a cause as you just pointed out. And that’s the thing that I think is so important for people to understand. If you can get to the root cause, oftentimes there are better answers than just treating symptoms. I’m living proof of this, and I know you have many, many patients who are as well, whether that be Lyme or mold, and I think that we’ll probably agree that these things all work together to torture you. One time I called Amy Proal last year and I was having some really weird symptoms. I’m like, I wonder if it’s my Lyme flaring or I just wonder if I’m dying. She goes, “Yeah. These infections live to torture you for your entire life, so don’t think you’re dying. This is just what they do. They just rise. They go back down, you treat them, you knock them down. This is just the nature of the beast.” And it can be super torturous. It can be really hard, but I do think they probably synergize in a very malicious way, ganging up on you.
Todd Maderis: I often say it is that perfect storm. I use the analogy of that it’s like having tacks in your foot. If someone walks in the door with a myriad of symptoms and they have six tacks in their foot and you find one, you find that they have Lyme, well, they still have five tacks in their foot, and you need to address all of them for them to recover. And when you asked me to come onto the podcast, I thought, well, what can I offer? I want to make sure that the listeners, there’s something that I have I could share, that people could benefit from. And I think about the strategy and the approach in treatment a lot. And I think that you could have multiple insults at the same time, but there’s a hierarchy in which you treat. And everyone is different.
“I think that you could have multiple insults at the same time, but there’s a hierarchy in which you treat. And everyone is different.”
– Todd Maderis
You’ll see this a lot on social media where someone will say, “Well, this therapy cured my Lyme, and so everyone else should try this therapy because it worked for me.” But ultimately, everyone is very different. I think about this—especially with these chronic Lyme clinics that we’re now seeing, and the research money that’s going into advanced chronic Lyme—ultimately, the studies are going to have to be very personalized and tailored. And that’s a challenge with the scientific method: we typically want to isolate variables. We want to study just Lyme. Well, you and I both know that ticks don’t carry just Lyme. In fact, the rule is they carry multiple infections, and it’s rare that someone gets just Lyme. So, if someone was tested by their pediatrician or their PCP and they had Lyme and they got doxycycline, well, it’s a high likelihood that they have a co-infection as well, and those require different antibiotics or treatments. So, it is complex, and I think the strategy is more, “We’re always looking for the treatment, the magic wand that’s going to make it all go away.” But it really begins with a thorough assessment. And then the treatment strategy is what I think even supersedes what we’re the magic treatment that we’re looking for down the road.
Dana Parish: One thing that I think would be great to dispel is this myth that there is no Lyme and there’s no tick-borne diseases in California. I can’t tell you how many times I continue to hear this from doctors and from patients. Kris Kristofferson didn’t get diagnosed for 30 years because he lived in Malibu.
By the way, people travel, but there’s Lyme in Malibu anyway. His doctors were just incredulous. And when I interviewed his wife, Lisa, about this—he famously had been diagnosed with Alzheimer’s—and then he went to an integrative doctor who tested him for Lyme. He had it. He had gone off the road. He couldn’t sing and perform anymore. Then he began treatment, and within a month (after a very serious decline), his wife said they were driving in the car—this was on the cover of Rolling Stone—and she said, “The son of a bitch is back!” The light was back! Back to being himself to some degree, and he was able to go back on the road and recover some. I don’t want to portray it as he had this miraculous 100% recovery because he didn’t. But he improved a lot when he was treated. But part of the problem was his doctors all thought that because he was living in California for so long and Hawaii, he couldn’t have Lyme, so they never even considered it.
Todd Maderis: And his profession was to tour.
Dana Parish: His profession was to tour. But isn’t it common where you are? You’re in Marin County, right?
Todd Maderis: I have a lot of thoughts around this and a couple of them come to mind. I just saw a study come out this week, I think from the CDC. It was the epidemiology of five tick-borne infections in the United States. And you look at the maps and they’re always a little dated, but when you do look at a map of the states, clearly there’s a major hotspot in the northeast, but the maps also include most of the west coast. And I know here in California, I think it’s 54 counties that we have Lyme? This is old stuff; these are data from probably 10 years ago. But Lyme has been found in ticks in like 42 out of the 54 counties, so we know it’s here. I always share what Dr. Bob Lane from UC Berkeley was doing in the 1970s. He was studying ticks back at the same time that Polly Murray discovered that the children had the outbreak in Lyme, Connecticut. He was studying ticks here in the coastal range of Northern California and finding pathogens in ticks, including ehrlichia and anaplasma. Lyme’s been on the west coast as long as it’s been in the northeast. This isn’t a new phenomenon, we only recognized it in the mid-1970s.
I think Mendocino County might have the highest incidences of infected ticks. Then we have Sonoma County, and then Marin County’s number three—Marin County happens to be a very active community. 80% of our county is preserved open space, so there’s a lot of hikers and bikers and equestrians. People are out and about. Then of course, a couple years ago there was this study about ticks being found on California beaches that were infected. So, it’s a real disservice when physicians don’t keep up with the literature. And of course, you can’t expect people to keep up with everything. We’re inundated with it. But back to the point I mentioned earlier about being curious and open-minded as more younger physicians come up and occasionally physicians train on the east coast, and so they did their residencies or fellowships on the East Coast. And so occasionally a patient will share that they went to the ER, and the doctor was familiar with Lyme and gave them a proper course of doxycycline. But ultimately, medicine is too vast to be dogmatic. You have to be open, and change takes time, but being open to the evidence itself that’s out there is the first step.
“Ultimately, medicine is too vast to be dogmatic. You have to be open, and change takes time, but being open to the evidence itself that’s out there is the first step.”
– Todd Maderis
Dana Parish: It’s surprisingly uncommon that doctors will even take these things into consideration when you tell them. That’s the thing that’s been so surprising for me, having dealt with chronic illness. I never expected not to be believed, somebody that goes in making up stories. I thought, “Of course those doctors will take me at my word.” Wrong. Absolutely not. When you come in with all these weird disparate symptoms, you get put in a psych bucket, or you get put in the anxious high-strung woman, hysterical bucket. It’s just very strange to be treated like that when you’re thinking, “Why would I make this stuff up?” You do wonder, too, about being treated like a psych case when you were having a brain infection, which wasn’t my case. We know that these infections and even these mycotoxins and metals and stuff can cause neuropsych symptoms. We know that they can have this basis. But what is the role of trauma separate from all these infections? Is there a role that trauma plays in chronic illness, and does it help to treat it?
Todd Maderis: Yes. Trauma can come from a number of different areas, and it’s not uncommon for me to see a new patient and I would say at least 50% of my patients will report some past history of trauma on their intake form. I might ask them about it, but they may or may not want to get into too much detail. But for a lot of my chronically ill patients, there is a past history—whether it’s psychological, physical, or sexual abuse. There have been a number of studies including the big ACE study, which was the Adverse Childhood Experience study, and we now know that the limbic system gets damaged. We basically developed neuronal pathways that help our survival, and it served us at one point in time, for example if you needed to run from the saber-toothed tiger, you are proficient at that.
Dana Parish: Can you describe what the limbic system is a little bit, just so people understand the importance of addressing this?
Todd Maderis: Yes. It’s the alarm center in the brain. It’s what goes off when the body senses there’s a threat and it could be anything. That creepy sensation that someone might get being around someone dangerous, it’s an alarm center and it’s a survival mechanism. But people later in life can also develop trauma from what you just described from being sick and gaslighting. My observation is that patients can develop trauma from not really being able to trust their own body.
You’ve heard this before where people say, “I don’t schedule lunches with my friends. I can’t plan to go on a hike on a Saturday because I don’t know what I’m going to get when I wake up in the morning.” And so, when you can’t trust your own body, then there’s a level of anxiety and uncertainty. The trauma can take many shapes and forms, but I do believe we know this with mast cell activation syndrome, for example, that stress can elicit a mast cell type of response. So, it keeps the body in a sympathetic dominant state. We’re supposed to have these short bursts of stress—not chronic stress—not waking up at 7:00 AM and getting in a car and commuting for an hour, or work that’s stressful. We’re supposed to have short bursts of stress, and our modern society unfortunately doesn’t support that very well. So, we have to be very proactive in taking care of ourselves and stress management, meditation, walking in nature, whatever it is that works for you. But over time, those neuronal pathways get so reinforced that people automatically go to that. And limbic retraining programs are where people can heal that limbic injury is the term that’s used.
Dana Parish: That’s interesting. So, what do people do? I have some friends that have done Dynamic Neural Retraining System DNRS. I haven’t tried to use these kinds of things, but I’m curious, is that a good program to try if this is one of the issues that’s plaguing you? Or are there other programs or other things people can do to sort of settle their nervous system, their limbic system, the fight or flight response?
Todd Maderis: Yes, absolutely. DNRS is one of them. Annie Hopper created that. And there’s the Gupta Program created by Ashok Gupta. Those are both online programs that people can do from their own homes. Eye Movement Desensitization and Reprocessing — EMDR— is an old technique that’s used with therapists, and that’s a form of limbic retraining. Neurofeedback and brain mapping are also very effective. Some patients are using ketamine now too. Ketamine can also help with neuroplasticity and help to retrain the brain. There’s a lot of tools out there. It’s a matter of finding one that works for you and one that’s going to be effective. But I do think for some people, like I mentioned earlier, every chronically ill person has their own makeup, their own fabric. And what percentage of the pie is trauma and what is infection and what is toxin? Everyone’s different. For some people, the past trauma plays a bigger role, or it keeps them stuck in a sick cycle. And that’s the hard part. I mean, something we haven’t talked about that I think is worth mentioning is—and I’ve had these conversations with other Lyme colleagues—where if it is a clear cut, chronic tick-borne infection case, you can put people on antibiotics and cycle through various antibiotics over time. Of course, we try to support other aspects of their healing, detoxification, immune system regulation, and people can get to a certain point, they might get 60%, 70% better, but they may never fully get back to their prior health.
 I think for clinicians, this is a conundrum. Why could we not get people better if there is a bug causing it, and we killed the bug? Why didn’t their health or their energy get back to normal or they’re painfully reduced? But some people are fine with it, they’re just pleased that they’re 70% better if they were hardly functioning prior to getting diagnosed. But there’s this healing aspect I’ve really begun to explore recently, and part of it has to do with the testing that I send to the German lab and then the treatment that we use. But there’s a healing cell membrane or cellular health that needs to occur. I always say it’s our cells what make up tissues. Our tissues are what make up organs and our organs of course make up our whole body. If oxidative damage is one of the main mechanisms of injury, we need to repair that damage. Because you’re only ever going to be as healthy as the health of your cells.
I think for clinicians, this is a conundrum. Why could we not get people better if there is a bug causing it, and we killed the bug? Why didn’t their health or their energy get back to normal or they’re painfully reduced? But some people are fine with it, they’re just pleased that they’re 70% better if they were hardly functioning prior to getting diagnosed. But there’s this healing aspect I’ve really begun to explore recently, and part of it has to do with the testing that I send to the German lab and then the treatment that we use. But there’s a healing cell membrane or cellular health that needs to occur. I always say it’s our cells what make up tissues. Our tissues are what make up organs and our organs of course make up our whole body. If oxidative damage is one of the main mechanisms of injury, we need to repair that damage. Because you’re only ever going to be as healthy as the health of your cells.
You cannot have a healthy organ that’s made up of unhealthy cells, whether it’s the heart or the brain or the muscles, the joints. I think that healing piece of the puzzle has been missing for so long. And there’s a mitochondrial researcher named Bob Naviaux who’s down at UC San Diego, and Dr. Naviaux has been in the chronic fatigue, ME/CFS and autism world and he’s been doing research for three decades. Recently, he wrote a paper describing how we need to change our approach to healing or recovery from chronic illness. It’s no longer the old model—what we call a pathogenesis or pathological model—where this was the cause, and we treat that and we move on. But with chronic illness, it’s very different. I heard him speak at a conference in 2019, and I went and dug up my notes from that conference and he had said, “The path from chronic illness back to health is not the same path that caused the chronic illness in the first place.”
And at the time I wrote it down it resonated with me. So, I took a note of that, but at the time it was like, “Well, what do you do with that?” Clinically, there’s always this gap. There’s research, there’s what we call bench medicine, and then there’s the clinician that shows up and maybe has limited time with their patients. How do we test for that? How do we treat that? And so that’s always been a missing piece of the puzzle, but I think we’re getting better at it now. I know that the tools that we’re using in my practice and what I’m seeing on follow-up testing and then what we’re hearing back from patients is we are helping them get closer and closer to that to complete healing. To me, that’s the most rewarding part. It’s not just getting them out of that acute state in their symptoms. How do we also help them prevent disease in the future? There’s no shortage of information in medicine, and if you’re interested and curious and you keep looking and digging, it’s very humbling actually.
Dana Parish: What do you think about food? What should people be eating? Is food playing a big role in people’s health?
Todd Maderis: Yes. Clearly, food is our fuel and Hippocrates said it’s our medicine as well. And if we put the right fuel in, your body pays dividends. Is there one perfect diet? I don’t think so. I think everyone’s a little bit different. There’s a lot of dogma out there around diet, and I often joke, I rarely talk about diet with my patients because the people I see have been chronically ill, and they’re so sick that when they walk in the door, they don’t say, “Yeah, I’m sick and I’m also eating McDonald’s every day. Right?”
They’re eating a really clean diet. I think a really good general diet is what we might call an anti-inflammatory type of diet. It’s avoiding foods that are common, inflammatory foods like gluten and dairy and sugar. And for some people, if they have a mast cell presentation, they might benefit from eating a low histamine diet. There’s the autoimmune protocol diet. There are a lot of various diets out there, but I think a plant-centric diet is really important. Very hypoallergenic, high dense nutrients, and there’s a number of ways to do it, but clean food is where it’s at. I think so much of our food supplies, of course, are sprayed and contaminated, you don’t want to be adding to your burden already.
Dana Parish: I agree. I’ve been madly tweeting about this for 24 hours because I’m back in New York now, and I did not know that New York City was now spraying pesticides from the back of a truck all throughout our residential neighborhoods in the city and in Queens. I only found out about it because some guy from Manhattan took a video of it. He’s sitting in his living room, 10:30 am, windows open, you and I know how these things aerosolize, and they go again, mycotoxin. They go way further in your little block and the street, they’re going into your apartment,
They’re adhering to your furniture. Again, talk about these pyrethroids. They stay in fabric for a long period of time. So, this guy takes a video, and you hear the police are leading them shouting with their megaphones, “Stay a hundred yards back, get in your apartment, close the windows. We’re spraying pesticides for West Nile virus.” There’s been about eight cases. Okay, so we’re doing nothing for Covid. We’re doing nothing to mitigate tick-borne diseases, but all of a sudden West Nile with eight cases, the entire city is sprayed with neurotoxic chemicals. And it just feels like it’s so hard to avoid. We have no choice. I don’t want this. I called the Department of Health multiple times yesterday to find out what exactly they were spraying. Are you going down my block or are you just mostly centering on the parks? Turns out that yes, they were going down my block between 2:00-4:00 am. I have a dog that had a very severe seizure from a pesticide/herbicide, and she’s severely averse to pyrethroids, and that’s what they were spraying. And I was like, well, a little warning would be nice! Some guy on Twitter shouldn’t be the one telling you “Go on our website.” Okay, well, I’m in the habit of going to your website to see what kind of horrible things you’re doing this week. And also, I have a little herb garden. So now my herbs, I feel are compromised. I’m trying to minimize; I do what I can. It’s expensive to be healthy. It’s expensive to buy organic foods, but I know that it’s important, so I do what I can and I’m like, now this happens!
Todd Maderis: First of all, I thought we stopped doing that in the 1970s, maybe early 1980s when they would spray. DDT has been banned, I want to say since the late 1970s in the US, but I’ve heard stories from patients over the years, and you’ve seen the famous photos of trucks and hot summer night in Texas, and they’re spraying DDT out the back and kids are running behind it because it’s hot and the spray is cool.
Dana Parish: I saw those pictures yesterday. People were posting them back to me complaining in New York saying, “This is what I grew up in. And we used to chase the trucks because it was fun to run through the cloud.”
Todd Maderis: Those are what we call persistent toxicants. And you can find those in people’s bodies 40 years later, the half-life is amazing. So, I didn’t realize that was even allowed at this point, but there’s something like 80,000 chemicals in daily use in the United States, and something like 200 of them have been tested on humans. So, we don’t know what the other 79,800 do to humans. Again, as we zoom out and we think about the patients listening to this and the chronically ill folks out there and maybe physicians and scientists that are also listening, and how do we help people? How do we get them better? What can we do to help them? And this is one of those areas that I think is grossly under-recognized. I’ll occasionally hear a physician that’s been practicing for 30 years say something like, “The patients I see now are much sicker than they were 15, 20 years ago.”
Why is that? Is it a rise in tick-borne infections or mold illness or environmental toxicants as well? It’s this perfect storm and to see people or their kids, or in their teens, or people in their early twenties with chronic fatigue syndrome and other neurological conditions, it’s just I think our environment is having a major impact on our health, and it’s really hard to get away from. If you’re inland or if your public health department is spraying right down your street, it’s very difficult to get away from. You could buy organic all day long—it’s very challenging.
Dana Parish: I was doing some research last night about how long these particles—pesticides and herbicides—stay aerosolized. There’s a Nature review that says three to 10 days. It can probably be hours depending on the wind, and we know a lot more about it, it’s more in the public domain now about air quality. I got really interested in this during the Covid pandemic because Covid is airborne, and we have to figure out how to protect ourselves. We have to learn a lot of stuff about air. I’m curious too, like you are, and I keep learning and I keep going down the rabbit hole and every time I go further, I’m like, “Oh, I don’t want to know! There’s nothing I can do.” But I should say one thing that I think is important is that when I first got Lyme and I was so sick before I could get to a doctor. There was a couple of weeks’ wait to get in.
Somebody put me in touch with a friend who had had a really severe case of Lyme that she recovered from. She told me, “If you don’t eat a paleo diet starting from today, don’t call me for help because you have to do something immediately to reduce inflammation.” It was such good advice. I’m not saying everybody will benefit from a paleo diet. I’m saying I did, and I really realized the importance of diet in that moment because I had a lot of physical pain, just aches and pains, fibromyalgia kind of stuff, joint pain. I would say that by the time I got to the doctor a couple of weeks later, having done very strict paleo in that period of time, my pain was reduced by 70%. I had a lot of other symptoms, but still, I’ll take it. I thought it was really incredible.
Todd Maderis: It’s profound, the effect that can have on our health and inflammation in the body. And sometimes we think about what I call the total body burden. It’s like a bucket, right? Everyone has a different size bucket, and we might have a different spigot at the bottom. Some people eliminate well, and others don’t. And once your bucket is full, if you sprinkle in a little, it could be anything. It could be gluten; it could be another pathogen. It just tips people over the edge. It could be perfumes, etc. Eating that clean diet doesn’t add to that burden that was already there. I think in general, when people are in a healthy state, they can eat a varied diet and not react to everything. But I see some people that can hardly eat anything at all, and whether that’s mast cell activation or leaky gut. I see a lot of my patients when we test them—because I’m a proponent of testing and using objective evidence—a lot of people have gut inflammation and treating that helps reduce their reactivity to things. I always say with something like a leaky gut, it’s not that the origin is in the gut, but the symptoms are systemic. So, it is headaches and brain fog and aches and pains and fatigue. If you reduce that—the inflammation that you’re putting into your body—you’re not going to trigger an immune response.
Dana Parish: Is there a good test for leaky gut?
Todd Maderis: There is, yes. There’s blood and stool testing for leaky gut.
Dana Parish: What are the tests called?
Todd Maderis: Well, there’s a lab called Cyrex that has a blood panel of leaky gut markers, and then there’s stool tests that also include a marker called zonulin. Anytime we order a stool test on patients, we always include zonulin because there’s an important connection. I often see leaky gut associated with things like SIBO (Small Intestine Bacterial Overgrowth) and even mast cell activation syndrome. They can all run in the same circle and be interrelated. Healing the gut is a critical part. 80% of our immune system is on the other side of your gut. Homebase to your immune system is right around your digestion. So, digestive health has an influence on your immune health. And when we talk about inflammation, we’re really talking about our immune system. Anything we can do to modulate the immune system improves (health) so it’s balanced. We always say the immune system wants to be like Goldilocks’s porridge. You don’t want an overactive inflammatory immune system or a weakened immune suppressed immune system. You want a just-right immune system.
Dana Parish: You just made me think of LDN. I think you might’ve been the first person to really talk to me about Low Dose Naltrexone—LDN, and it’s been a hot topic lately because a lot of Long Covid patients have stumbled upon it. This is something Lyme patients have been taking for a long time and probably many, many others. Tell us a little bit about LDN and have you had a lot of experience using it with your patients? What has it been like?
Todd Maderis: Yes. I love LDN. I think it’s probably one of the best tools in my toolbox. Naltrexone is also manufactured as a drug in 50 milligrams for alcohol and drug addiction. And it’s a medication that’s been around since the 1960s, I believe. But in the early 1980s, some doctors in New York started using low doses of it with AIDS patients to help keep them alive. They were using very low doses—like a milligram or so—and in low doses, the naltrexone is what is called a partial opiate antagonist. It partially blocks opiate receptors and then your body makes more endorphins, and so that helps to modulate the immune response. It reduces inflammation, it even helps with brain inflammation, but I use it when there’s gut inflammation as well. I mean, any autoimmune condition, I guess shouldn’t give medical advice, but I think most autoimmune conditions would benefit from LDN.
Dana Parish: I think so because I hear it all the time.

Todd Maderis: Neurological conditions, MS, Parkinson’s, all of those neurodegenerative conditions really, really benefit from LDN and it has to be dosed correctly. I always start with a milligram. I used to start with 1.5mg, and then you increase the dose each week up to, it used to be up to 4.5mg. I now start patients on a milligram, have patients increase a milligram each week up to 4mg. I’ve had better success with that. I think patients tolerate it better. One of the more common side effects is it can affect the patient’s ability to fall asleep. If that happens—because you typically take it at bedtime—I just have patients take it in the morning,
Dana Parish: People have wild dreams on it. There’s a case of someone who had a 9-11-related smell and taste disorder, tried many, many, many things. And LDN seems to be the best drug or the best therapy that he’s landed on to help his smell and taste. And again, there’s lots of emerging research in the advent of Covid with a lot of unknowns here, but I haven’t heard too many people talking about that, but I thought that was super interesting.
Todd Maderis: Yes, it’s a great medication for all the conditions we’ve discussed today. There’s an application of LDN there.
Dana Parish: There’s a great little book. I think it’s actually called the LDN Handbook or something like that. I read it and I thought it was a really interesting, quick, easy read, and it gave me a good overview of the things people were using it for, cancer and all kinds of other stuff. And it’s really safe and easy to tolerate for most people.
Todd Maderis: Yes. It has very few side effects. It has a long track record of being an effective, safe medication. I wrote an article on my website about LDN, the use of LDN for Lyme disease, chronic Lyme, and I put a lot of the research in there around how it would benefit people with Lyme. So, it’s an amazing medication. Of course, it has to be compounded because it’s used in low doses. Some people try to get a 50-milligram tablet and then make their own dose, and I don’t recommend that. I think you really want it compounded in a precise dose, and that’s where you’re going to get the most benefit.
Dana Parish: That makes sense. Since we’re on the topic of LDN and Long Covid, are you seeing Long Covid in your practice now with complex chronic illness? How is it impacting people? Are there some strategies that you’ve landed on that have been helpful? I mean, it’s interesting to go to somebody like you because you know a lot about chronic infections already, and most doctors are completely at a loss when it comes to chronic infections driving chronic illness. So, I would think you would be a natural go-to person for Long Covid issues.
Todd Maderis: I think any physician that was treating chronic infections like Lyme disease or chronic viral infections was pretty well-positioned to treat Long Covid. But we’ve all realized that it’s a very challenging condition and there’s still a lot that we don’t know about it. There have been theories since three to six months into Covid. We were theorizing why some people had persistent symptoms—from autoimmune to cytokine storm to triggering mast cells to viral reactivation— there have been a number of theories. I often say I’ve yet to meet a Long Covid patient that didn’t have something else going on. It’s like that “tack in the foot” analogy I used earlier, and whether they knew it or not, that’s the thing when people say, “He was perfectly healthy until he got XYZ,” and that may be the case. There may be those patients out there, the folks that I’ve seen when we cast a broad net with tests and figure out what else is contributing to that total burden. And when we run other tests, they may have other infections, or they may have high mycotoxin levels that are suppressing their immune system. It’s like that perfect storm that happens.
We know this virus can persist in people’s bodies now, and so that may factor in as well. It’s really clear that no one’s cracked the code. If we had, then there wouldn’t be however many millions of people walking around right now with Long Covid. I’ve been looking at cellular damage that can occur from any chronic exposure and then applying the treatment that we use to help repair that. Because again, to Dr. Naviaux’s point that the road from chronic illness back to health is not the same path that caused it. So, if it is viral persistence and we just put someone on an antiviral, for example, are they going to fully recover?
Dana Parish: Are you finding benefits using antivirals? We know, as you mentioned, Covid can activate latent infections like Epstein-Barr Virus EBV. Also, Lyme. We’re seeing it a lot in vector-borne diseases. They are reactivating people that were in remission or recovered and they have the same symptoms again after they got Covid. What can you do about that?
Todd Maderis: Well, 90% of people walking around have elevated IgG antibodies to Epstein-Barr because nine out of 10 of us have been exposed in childhood.
So, what is reactivation? Is it just a high IgG titer or if you see an IgM, Epstein-Barr viral titer, you want to treat that for sure. I use T-cell testing in my practice for these chronic viruses and T-cells will only be elevated with an active infection. If I have an EBV positive T-cell test, then I’m absolutely treating that. But to answer your question around reactivation of things or are we using antivirals? For sure. It really ends up being that perfect storm and you have to assess everyone individually and figure out what their makeup is, what they need and what’s the hierarchy, the strategy in getting them better. What is it going to look like going forward? I don’t know. I guess the future will tell, but right now using all the tools that we use with other chronic illnesses, I think is really the most effective way to help people.
I have a patient right now who I had treated years ago for Lyme and Bartonella, and she’d recovered and was living a fairly normal life. And then she got Covid—we think maybe one of the earlier cases of Covid. And she has been so sick since that happened. I mean, when I see her, she’ll say, “Chronic Lyme was nothing compared to what I’m going through now.” And she has an autoimmune encephalitis picture, and so she has a lot of brain inflammation and we’re trying to use a therapy called IVIG for her. And yes, it is messy out there, but I’m optimistic that a lot of the tools that we’ve used historically are what really help move people in the right direction.
Dana Parish: I am seeing some people getting benefit on things like LDN, hyperbaric oxygen, tools that we’ve learned that have helped patients in the Lyme world. They seem to be applicable to some degree with these other issues. Well, I can’t thank you enough. First of all, time has flown. We have to do part two! We still have a lot of ground cover. I’m so happy that you came on. Did I miss anything? Is there anything that you wanted to cover before we left or did we cover?
Todd Maderis: We covered a lot. I love this. Thank you so much for having me. It’s an honor, and I could talk about this stuff all day long. I really enjoy the work that we do. I’m grateful for organizations like Bay Area Lyme and people like yourself that have put out great information or been outspoken about these conditions because we physicians are on the frontline. I always say my obligation is to the person that’s sitting across from me in my office, to help them get better, and despite what the CDC guidelines are or whatever else it may be, my job is to get the patient better. So, I appreciate all the work that groups like yourself and Bay Area Lyme and lymedisease.org are doing. There are wonderful groups out there. So, thank you for all the great work that you do.
Dana Parish: Thank you so much for saying that. Where can people find you and where can people learn more about you and read your great articles that you publish?
Todd Maderis: Well, my website is Dr. Todd Maderis and just Google it and it’ll pop up. I haven’t written much lately on that site, but we do post a lot of research on my Instagram account, which is Dr. Todd Maderis, and also I’m on Twitter, and I think that’s Dr. Todd.
Dana Parish: Great. Well, we will continue our conversation. Thank you so much for this. This has been awesome and wonderful, and you’re going to help a lot of people. Thank you.
Todd Maderis: Thank you for having me.
This blog is part of our BAL Spotlights Series. It is based on a transcript from Ticktective, our podcast and video series. To listen or watch the original conversation, please click here. Bay Area Lyme Foundation provides reliable, fact-based information so that prevention and the importance of early treatment are common knowledge. For more information about Bay Area Lyme, including our research and prevention programs, go to www.bayarealyme.org.
